Trends in Oncology
How Radioisotopes Are Being Used to De-Risk Antibody-Drug Conjugate (ADC) Development
Antibody-drug conjugates (ADCs) continue to generate momentum in oncology, offering the promise of targeted cytotoxic delivery with greater specificity and reduced systemic toxicity. However, the complexity of these molecules, from antigen binding and internalization to payload release and clearance, makes them notoriously difficult to optimize. Many ADC programs stall not because the payload is ineffective, but because developers lack insight into whether the antibody is reaching and engaging the target in vivo. Radiotracers offer a unique opportunity to bridge this knowledge gap. By radiolabeling antibodies, , or ADC-like constructs with radioisotopes, researchers can evaluate in vivo biodistribution, tumor targeting, and off-target accumulation long before clinical trials. These tools provide a non-invasive, high-resolution view of compound behavior that traditional pharmacokinetic assays or histology cannot capture alone. In this article, we explore how radiotracers techniques, when combined with clinically relevant preclinical models, are helping ADC developers de-risk critical decisions earlier in the development cycle. From model selection to target validation to biodistribution profiling, radiotracers are becoming an indispensable part of the ADC toolkit. PDX Models + Radiopharmaceuticals = Translational Power Understanding Risk in ADC Development The appeal of ADCs lies in their elegant concept: deliver a cytotoxic payload directly to cancer cells via a highly specific antibody, sparing healthy tissue. In practice, however, ADC development is fraught with failure points. Many candidates show limited efficacy or unacceptable toxicity — not due to poor payload design, but because of incomplete understanding of how the construct behaves in vivo. Key risks include: Heterogeneous or insufficient target expression, which leads to poor tumor uptake Off-target accumulation in antigen-expressing normal tissues Suboptimal pharmacokinetics, including premature clearance or payload release Lack of internalization or poor intracellular trafficking, reducing payload delivery These risks are difficult to detect with traditional in vitro methods alone. Even when early pharmacology data appear favorable, translational failures often emerge when the compound enters more physiologically complex systems or encounters unexpected biological variability. What ADC developers need is a translational lens into antibody behavior — one that captures how the full construct distributes across tumor and normal tissue, how long it persists at the target site, and how that behavior varies across models. That’s where radiotracers come in. Radiolabeling ADCs to Visualize Biodistribution and Target Engagement Radiolabeling ADCs with radioisotopes enables developers to evaluate compound behavior with far greater granularity than traditional methods. By tagging the antibody or the full ADC construct with an isotope such as Zirconium-89 (Zr-89), Lutetium-177 (Lu-177) or Indium-111 (In-111), researchers can track distribution, uptake, and retention across tissues and tumor models in real time. This technique serves multiple functions: Biodistribution profiling: Understand where the antibody accumulates, and how much it localizes to the tumor versus healthy organs Target engagement assessment: Confirm that the biologic is reaching antigen-positive tumors with sufficient intensity and duration In vivo tumor targeting characterization in well characterized PDX models: Understand ADC distribution variability across PDX with preserved inter- and intra-tumoral heterogeneity found in human cancers. Off-target surveillance: Identify unintended uptake in antigen-expressing normal tissues (e.g., liver, spleen, bone marrow) early in development (depending on cross reactivity) Comparative evaluation: Screen multiple antibodies, formats, or linkers to determine which offers the best tumor-to-background ratio Radiolabeled ADC constructs can be studied across multiple timepoints to assess dynamic distribution and clearance profiles. When paired with well-characterized preclinical models—particularly those that reflect human heterogeneity in target expression, this approach allows for an evidence-based refinement of lead selection and study design. In addition to guiding compound optimization, radiolabeled compounds generate data that supports IND-enabling work by illustrating tumor specificity and helping predict potential toxicity risks related to off-target delivery. Using PDX Models to Reflect Real-World Variability in Antigen Expression While radiolabeling provides a powerful tool for visualizing distribution, the choice of model system ultimately determines how meaningful those insights will be. Cell line–derived xenografts (CDX), though commonly used, often overexpress the target antigen in a uniform and artificial manner. This can mask important limitations in targeting specificity and distribution, leading to false confidence in a compound’s performance. In contrast, patient-derived xenograft (PDX) models preserve the inter- and intra-tumoral heterogeneity found in human cancers. Differences in antigen density, vascularization, stromal composition, and tumor architecture all impact how an ADC or radiolabeled construct will behave in vivo. Testing compounds across a panel of PDX models allows developers to assess performance across a range of real-world tumor phenotypes, gaining visibility into variability that may influence clinical response. Champions Oncology’s Lumin platform includes hundreds of PDX models annotated with genomic, phenotypic, and treatment-response data. These models can be screened in advance using tissue microarrays (TMAs) to identify tumors with varying levels of antigen expression, enabling strategic model selection and rational study design. In the context of radiopharmaceuticals or radiolabeled ADCs, this means developers can: Evaluate targeting across low, mid, and high-expressing tumors Identify models most likely to mirror patient response Explore relationships between uptake and known molecular drivers By integrating radiolabeling with clinically annotated, heterogenous models, developers gain a more complete picture of how a compound is likely to perform across the clinical population —and avoid late-stage surprises. From Imaging to Strategy: De-Risking ADC Development Earlier in the Pipeline The high cost and complexity of ADC development demand early, informed decision-making. Traditional pharmacology and histology provide critical insights, but they don’t tell the whole story, especially when it comes to understanding how a biologic behaves in real biological systems over time. Radiotracers tools fill that gap by enabling non-invasive, temporal, and quantitative evaluation of ADC behavior across diverse, clinically relevant models. When used early in development, radio labeling and biodistribution studies can help developers: Select better antibody constructs or formats based on real in vivo performance Prioritize linker-payload combinations with favorable pharmacokinetics and tumor retention Predict potential toxicity or dosing issues from off-target accumulation Justify model selection and dose rationale in regulatory submissions By integrating these insights into the design phase — not as a retrospective check — developers can refine their therapeutic strategy while reducing attrition risk later in the pipeline. Radiotracers not only illuminate compound behavior but also serve as a translational bridge that connects target biology, delivery, and clinical feasibility. In a field where timelines are long, investment is high, and failure is costly, this approach offers a pragmatic and data-rich path forward: study smarter, screen earlier, and develop with confidence. The Only CRO Pairing PDX Models with Radiopharma
.jpg)
Why PDX Models Are Essential for Radiopharmaceutical Testing
Radiopharmaceuticals represent a rapidly advancing class of targeted oncology therapeutics, leveraging radionuclide-labeled molecules to deliver ionizing radiation directly to tumor cells. Despite the promising clinical potential of alpha- and beta-emitting radiopharmaceuticals, achieving translational success remains challenging. Robust, well-characterized preclinical models are essential to increase confidence in compound performance before entering the clinic. Where biodistribution, receptor heterogeneity, and tumor penetration critically influence therapeutic index and patient selection strategies, traditional preclinical models often fall short. Cell line–derived xenografts (CDX), in particular, offer limited predictive value due to their clonal homogeneity, uniform tumor architecture, and lack of biological diversity, factors that can lead to inaccurate assessments of targeting performance, distribution, and treatment efficacy. Patient-derived xenograft (PDX) models offer a superior alternative, retaining the histological architecture, molecular diversity, and intra, and inter-tumoral heterogeneity of the donor patient’s tumor. These attributes enable more physiologically relevant assessment of targeting efficacy, radiotracer distribution, and therapeutic response—key metrics in determining compound viability prior to clinical translation. In this article, we examine the limitations of traditional models, the biological advantages of PDX platforms, and the specific ways in which PDX enhances radiopharmaceutical study design. We also highlight how access to large, clinically annotated model libraries—such as Champions Oncology’s Lumin platform can support more informed, data-driven decisions during preclinical development. PDX Models + Radiopharmaceuticals = Translational Power The Limits of Traditional Preclinical Models Despite their ubiquity in oncology research, traditional preclinical models—particularly cell line–derived xenografts (CDX)—present significant limitations for targeted drug development, including radiopharmaceuticals. CDX models are generated by implanting immortalized cancer cell lines into immunodeficient mice. While they offer logistical advantages such as rapid tumor growth and reproducibility, these models are inherently reductionist. Their clonal architecture lacks the genomic and phenotypic heterogeneity observed in primary tumors, which can lead to misleading conclusions regarding target accessibility, tumor penetration, and intratumoral uptake of radiolabeled compounds. Moreover, CDX models typically fail to recapitulate the complex tumor microenvironment (TME), including stromal interactions, vasculature, and immune contexture—all of which are known to influence radiopharmaceutical distribution and efficacy. In addition, receptor expression in cell lines is often artificially uniform or overexpressed, providing an inaccurate representation of clinical target variability. For radiopharmaceuticals — where therapeutic performance depends heavily on fine, tuned targeting, localized retention, and clearance kinetics, these simplifications are not benign. Data generated from CDX models may overestimate therapeutic potential or fail to predict safety liabilities, contributing to a translational gap between preclinical validation and clinical outcomes. What Makes PDX Models Different Patient-derived xenograft (PDX) models are established by implanting primary tumor tissue directly from oncology patients into immunodeficient mice, preserving the cellular heterogeneity, stromal components, and histopathological architecture of the original tumor. Unlike CDX systems, PDX models retain critical aspects of human tumor biology across multiple passages. This biological fidelity translates into substantial advantages for radiopharmaceutical development. First, PDX models capture both intratumoral and intertumoral heterogeneity, a key determinant of response variability in radiolabeled therapies. Differences in antigen density, receptor expression, vascularization, and stromal composition can significantly affect radiotracer uptake and therapeutic distribution—elements that are often uniform or absent in traditional systems. Second, because PDX tumors grow in vivo without prior dissociation or in vitro manipulation, their tumor microenvironments more accurately reflect the spatial and structural complexity of human malignancies. This includes irregular vasculature, hypoxic regions, and heterogeneous interstitial pressure—factors that influence compound diffusion, radiation deposition, and biological effects. PDX models have demonstrated greater predictive validity than CDX systems across multiple drug classes, with treatment responses that more closely reflect clinical outcomes. This makes them particularly valuable for de-risking radiopharmaceutical assets in the early stages of development, providing insight into variability in target engagement and therapeutic effect. While tumor-specific uptake can be assessed in a human-relevant context, off-target distribution in preclinical models may not fully reflect human cross-reactivity due to interspecies differences in antigen expression. In short, PDX models offer a translational bridge between mechanistic discovery and clinical decision making, one that is especially important when developing complex, spatially dependent therapies like radiopharmaceuticals. How PDX Enhances Radiopharmaceutical Testing The evaluation of radiopharmaceuticals requires more than evidence of cytotoxicity; it demands a nuanced understanding of how a radiolabeled compound distributes within and interacts with—a tumor and its microenvironment. PDX models provide the translational resolution needed to interrogate these complex dynamics. One of the primary advantages of using PDX models in this context is the ability to model inter-patient variability in target expression. Radiopharmaceuticals often rely on the presence of specific cell surface antigens or receptors for tumor localization. In a clinical setting, these markers are rarely expressed uniformly across patient populations. By leveraging a library of diverse PDX models—each with distinct molecular and phenotypic profiles—researchers can assess how differences in target expression influence uptake, specificity, and efficacy. Additionally, PDX models enable realistic biodistribution analysis in tumors that replicate human heterogeneity in vascular density, stromal content, and perfusion. These factors play a significant role in modulating the intratumoral deposition of radiolabeled compounds, Preclinical studies in PDX therefore allow developers to anticipate challenges related to tracer penetration, off, target accumulation, and clearance kinetics, challenges that CDX models routinely obscure. Efficacy evaluation is another area where PDX models offer substantial value. Because these tumors respond to treatment in ways that reflect clinical patterns, including partial response, acquired resistance, and heterogeneous regression, they offer a more realistic basis for determining therapeutic window, optimal dosing, and potential biomarkers of response. When used systematically, PDX models allow radiopharmaceutical developers to move beyond binary efficacy readouts and instead generate layered, clinically relevant insights into compound behavior—insights that inform both development decisions and regulatory discussions. The Lumin Advantage While the value of PDX models in radiopharmaceutical development is clear, the ability to scale these insights depends on access to a diverse, well-characterized model library. Champions Oncology’s PDX platform is the most deeply annotated and clinically relevant PDX collections available globally, enabling sponsors to tailor studies with unprecedented precision. The library encompasses thousands of PDX models derived from a wide range of solid tumors, each backed by comprehensive clinical, histological, and molecular data. This includes mutational profiles, gene expression signatures, prior treatment history, and, critically for radiopharmaceutical programs, data on target expression heterogeneity across tumor types. To accelerate the design of rational studies, complementary tissue microarrays (TMAs) prepared from the PDX collection are also available. These arrays allow researchers to screen panels of models for antigen expression or biomarker prevalence prior to initiating in vivo work, enabling efficient model selection, improving study design, and reducing downstream variability. In radiopharmaceutical testing, where variability in receptor density or antigen availability can dramatically influence tracer uptake and therapeutic effect, this level of pre-screening and data integration is a strategic advantage. It allows developers to assess compound performance across diverse biological backgrounds and identify model subsets most likely to inform clinical translation. Combined with Champions’ in-house imaging, conjugation, and radiolabeling capabilities, Lumin platform offers a comprehensive ecosystem for generating radiopharmaceutical data that’s not only robust—but truly relevant to human disease. The Only CRO Pairing PDX Models with Radiopharma

Beyond TCGA: TumorGraft’s New Frontier in Cancer Research
Imagine a world where doctors can predict how a tumor will respond to treatment before a patient starts therapy. For decades, cancer researchers have relied on The Cancer Genome Atlas (TCGA), a massive dataset of 20,000 samples across 33 cancer types, to decode the molecular secrets of tumors. But TCGA has a blind spot: it mostly studies untreated, primary tumors, leaving critical questions about advanced cancers and treatment responses unanswered. Enter the Champions Oncology TumorGraft® platform—a game-changer in cancer research. With 1,500 patient-derived tumor models from over 50 cancer types, TumorGraft® captures the real-world complexity of advanced, metastatic, and heavily treated tumors. By combining molecular data with detailed pretreatment histories and treatment response insights, it’s opening new doors for predicting drug effectiveness, uncovering resistance mechanisms, and designing smarter therapies. In this post, we’ll explore how TumorGraft® complements TCGA, using a fascinating case study on mutational signatures to show its power. TCGA: The Gold Standard with Limits TCGA is a cornerstone of cancer research. It's publicly accessible, high-quality data, spanning DNA, RNA, and proteins, has fueled countless discoveries about how tumors develop. Researchers use it to characterize tumors, improve diagnoses, and identify molecular drivers of cancer. But TCGA isn’t perfect. Most of its samples come from primary, untreated tumors, with only a small fraction (about 42 patients) having received neoadjuvant treatment. This makes TCGA ideal for studying cancer’s early stages but less useful for advanced, metastatic, or post-treatment tumors. It also underrepresents certain populations and cancer stages, lacks pretreatment histories, and doesn’t allow access to physical samples for follow-up experiments. If you’re studying treatment resistance or real-world patient outcomes, TCGA’s data can only take you so far. TumorGraft®: A Window into Advanced Cancers The TumorGraft® platform, developed by Champions Oncology, flips the script. Its 1,500 patient-derived xenografts (PDXs)—tumors grown in mice to mimic human cancer—represent over 50 cancer types, focusing on advanced-stage, metastatic, and pre-treated tumors. These models reflect the diversity and complexity of patients seen in clinics, where cancers often evolve under the pressure of multiple therapies. Unlike TCGA, TumorGraft® includes detailed pretreatment information, capturing the therapies patients received before their tumors were sampled. This data, which can be further mined, offers a window into how prior treatments shape tumor biology, enabling researchers to study real-world clinical scenarios. Combined with treatment response data from in vivo experiments, where Champions Oncology has tested drugs representing multiple standards of care and measured Tumor Growth Inhibition (TGI)—how much a drug slows tumor growth—TumorGraft® unlocks use cases TCGA can’t touch: • Predicting Treatment Responses: See how a tumor’s molecular profile and pretreatment history predict its reaction to specific drugs. • Discovering Biomarkers: Identify markers that signal whether a treatment will work, informed by prior therapies. • Understanding Resistance: Study why some tumors resist therapy and find ways to overcome it, leveraging pretreatment data. • Improving Combination Therapies: Test drug combinations to find the most effective mixes, considering treatment histories. • Finding New Drug Targets: Link molecular features and pretreatment patterns to treatment outcomes to uncover novel therapies. Mutational Signatures: A Shared Language To prove TumorGraft’s® reliability, researchers compared it to TCGA using mutational signatures—DNA damage patterns that act like fingerprints, revealing what caused a tumor, like UV light or faulty DNA repair. These signatures, cataloged in the COSMIC database, help identify vulnerabilities in tumors and guide treatment strategies. The analysis began by curating COSMIC signatures and calculating their exposure and frequency in both TCGA and TumorGraft® datasets. Figure 1: Diagram showing calculated exposure/frequency of tumors in TumorGraft® (left) and TCGA (right). The results were striking. Both datasets flagged similar patterns. For example, SBS7a—a signature tied to UV light exposure (COSMIC SBS7a)—was strongly linked to melanoma in both TumorGraft’s® PDX models and TCGA’s samples. Analysis of 1,155 PDXs revealed SBS7a as a hallmark of melanoma, mirroring TCGA’s findings. This alignment shows that TumorGraft’s® data is as biologically accurate as TCGA’s, despite its focus on advanced, treated tumors. Figure 2: Chart of multi-omic data analysis from 1,155 TumorGraft® PDXs, highlighting trends in mutational signatures across tumor types. Figure 3: Bar chart showing SBS7a mutational signature prevalence in melanoma PDXs from TumorGraft®, with high association compared to other cancer types. Researchers analyzed signatures using different motifs—single base substitutions (SBS96), double base substitutions (DBS78), and insertions/deletions (IND83). All signatures found in TumorGraft® appeared in TCGA, with TCGA’s larger sample size revealing a few extra patterns due to its scale. Figure 4: Comparison of mutational signatures across SBS96, DBS78, and IND83 motifs in TumorGraft® and TCGA datasets. A UMAP plot, a visual tool that maps data similarity, confirmed that tumors cluster by type (e.g., melanoma, lung), not by whether they came from TCGA or TumorGraft®. This suggests that biology, not the data source, drives the differences—a green light for using TumorGraft® alongside TCGA. Figure 5: UMAP scatterplot showing tumors clustered by type, not data source, confirming TumorGraft’s® biological consistency with TCGA. Figure 6: Dot plot showing associations between mutational signatures and metadata, with dot size indicating event frequency and color representing p-value. Notably, tumors with signatures SBS6, SBS15, and SBS10b showed resistance to alkylating agents and platinum-based chemotherapies, exhibiting lower TGI. According to COSMIC, SBS6 and SBS15 are linked to defective DNA mismatch repair, common in microsatellite-unstable tumors, while SBS10b is tied to mutations in DNA polymerase epsilon, often seen in hypermutator tumors. By mining pretreatment data, researchers can explore how prior therapies influence these resistance patterns, offering clues to personalize treatments and avoid ineffective drugs. Figure 7: Graph showing correlation between SBS6, SBS15, and SBS10b signatures and resistance to alkylating agents/platinum in TumorGraft® PDXs, with lower tumor growth inhibition (TGI). This is just the beginning. TumorGraft’s® pretreatment data, combined with patient treatment histories and in vivo responses to thousands of standard-of-care drugs, is a goldmine for studying how prior therapies shape tumor evolution and treatment outcomes. Why TumorGraft® Matters The similarities between TCGA and TumorGraft’s® mutational signatures prove that TumorGraft® is a reliable partner to the gold standard. But its focus on advanced, treated tumors, detailed pretreatment information, and treatment response data takes cancer research to new heights. The ability to mine pretreatment histories—unavailable in TCGA—enables researchers to uncover how past therapies influence tumor biology, paving the way for personalized medicine and better patient outcomes. Whether you’re developing new drugs, tackling treatment resistance, or designing combination therapies, TumorGraft® provides insights that TCGA can’t. Looking ahead, researchers can dig deeper with TumorGraft® by exploring copy number signatures, RNA sequencing, or proteomics. Mining pretreatment data alongside these analyses could reveal even more about how tumors evolve under therapeutic pressure, driving breakthroughs in cancer care. Ready to Transform Cancer Research? The TumorGraft® platform is more than a dataset—it’s a bridge to personalized medicine. By combining the molecular depth of TCGA with TumorGraft’s® real-world treatment and pretreatment insights, researchers can unlock answers that bring us closer to curing cancer. Want to explore TumorGraft® for your next study? Learn how our platform can power your research today. Note: Data sourced from Champions Oncology and validated against TCGA’s data using the mutational motifs in COSMIC.
Predicting ADC Efficacy Using IHC and NGS
Antibody-drug conjugates (ADCs) represent a cutting-edge advancement in cancer therapy. These unique biopharmaceuticals act as "smart bombs," combining monoclonal antibodies specifically targeting cancer cells with potent cytotoxic drugs delivered directly to the tumor site. This precise targeting reduces collateral damage to healthy cells, minimizing adverse effects. Given the growing adoption of ADCs in clinical oncology, predicting their efficacy has become a critical challenge. Factors such as tumor heterogeneity, antigen expression, and individual patient differences underscore the need for precise biomarkers and advanced tools to determine patient suitability. The integration of immunohistochemistry (IHC) and next-generation sequencing (NGS) has emerged as a powerful approach to refining this prediction process. This blog explores the challenges of predicting ADC efficacy, the roles of IHC and NGS, and how these technologies are shaping the future of ADC-based therapy. The Importance of Predicting ADC Efficacy Why Predicting ADC Outcomes is Crucial? The therapeutic landscape of ADCs continues to evolve, with several FDA-approved ADCs and many others progressing through clinical trials. However, not all patients with cancer respond to these therapies, making the prediction of ADC efficacy vital to ensuring optimal outcomes. Key considerations include: • Target Antigen Expression: ADCs' performance depends on the presence and density of specific antigens on tumor cells. • Tumor Heterogeneity: Variability in antigen expression within and between tumors can impact ADC penetration and effectiveness. • Resistance Mechanisms: Both primary and acquired resistance to ADCs challenge their sustained efficacy. The Role of Immunohistochemistry in Predicting ADC Efficacy How IHC Works in ADC Therapy? Immunohistochemistry (IHC) is a gold standard for detecting protein expression within tumors. By applying antigen-specific antibodies to tissue samples, IHC enables visualization and quantification of target antigens. For ADCs, this method is highly valuable in determining whether a patient’s tumor expresses the antigen necessary for ADC binding and delivery. Benefits of Using IHC for ADC Target Assessment • Direct Visualization: Precise localization of target antigens not only confirms presence but also identifies antigen distribution within the tumor. • Threshold Analysis: IHC enables clinicians to set expression thresholds for ADC targeting, ensuring that only eligible patients receive therapy. • Readily Available Tool: IHC is widely accessible across pathology labs, making it a practical option for many cancer centers. Challenges in IHC Analysis Quantification of protein expression in IHC is typically assessed with H-scores, calculated by pathologists based on the identification of the percentage of cancer cells expressing the target and its level of intensity. The subjectivity of the methodology is an inherent risk of inconsistency for inter- intra- assay, for this reason, the H-score is usually calculated as the result of the independent IHC data analysis from at least two pathologists. Also, despite its benefits, IHC has limitations in predicting ADC efficacy, as for known ADC targets such as HER2 and TROP2, the correlation between target expression-related IHC scores and ADC efficacy, is not always strong. Next-Generation Sequencing (NGS) Contributions to ADC Accuracy What is NGS and How it enhances ADC Targeting? Next-generation sequencing (NGS) analyzes DNA, RNA, and gene expression at unprecedented speed and precision. By providing data-rich insights, NGS enables oncology researchers to evaluate molecular profiles in addition to traditional methods like IHC. In particular, NGS data can help researchers with the identification of biomarkers that may predict ADC responses. Recent studies have demonstrated NGS's advantages in ADC biomarker identification. For example, RNA sequencing correlations with IHC staining (e.g., TROP2, HER2) highlight strong alignment in certain targets, offering the potential for RNA-based cutoffs to complement IHC in ADC prediction. Variability, however, remains for some antigens, underscoring the need for continuing refinement. Innovations in Predicting ADC Efficacy Beyond IHC and NGS Emerging technologies and methodologies are refining ADC efficacy prediction even further. Key innovations include: • Multivariate Biomarkers: Next-gen tools like ADC Treatment Response Scores (ADC-TRS) evaluate gene expression alongside additional factors (e.g., adhesion, proliferation markers), significantly enhancing response prediction. • AI-Powered Pathology: Artificial intelligence in cancer pathology is enabling automated image and molecular data analysis, providing deeper insights into tumor heterogeneity and antigen expression thresholds. • Molecular Imaging: Imaging technologies are being integrated with NGS and IHC to provide real-time visualization of ADC biodistribution within patient tumors. Future Potential • Predictive Precision: Enhanced tools and algorithms will improve patient stratification, leading to better survival outcomes and fewer treatment-related toxicities. • Adaptive Therapies: With the ability to monitor antigen dynamics over time, clinicians can tailor ADC therapies to evolving tumor characteristics. Accurate Predictions Mean Better Outcomes for Patients Antibody-drug conjugates are paving the way for highly targeted and effective cancer treatments. However, maximizing their potential hinges on the ability to accurately predict suitable candidates through methods like IHC and NGS. By leveraging the latest advancements in predictive biomarkers and sequencing technologies, scientists and oncologists can improve patient outcomes, advancing precision medicine to new heights. As the field evolves, innovations will continue to refine ADC efficacy predictions, enabling personalized treatment strategies that benefit patients across diverse cancer types. Reach out to Champions Oncology to learn more about how we can help you develop your ADCs with our cutting-edge ex vivo and in vivo platforms and predictive tools that drive innovation. [1] Katrini J, Boldrini L, Santoro C, Valenza C, Trapani D, Curigliano G. Biomarkers for Antibody-Drug Conjugates in Solid Tumors. Mol Cancer Ther. 2024 Apr 2;23(4):436-446. doi: 10.1158/1535-7163.MCT-23-0482. PMID: 38363729. [2] Sachdev P. Thomas, Laurel A. Habel, Jennifer Marie Suga, Ninah Achacoso, Josh Nugent, Katarina M. Robinson, Ryan White, and Scott A. Tomlins. Evaluation of a predictive biomarker for antibody drug conjugates (ADCs). Journal of Clinical Oncology, Volume 42, Number 16_suppl. doi.org/10.1200/JCO.2024.42.16_suppl.3140 [3] Makawita S, Meric-Bernstam F. Antibody-Drug Conjugates: Patient and Treatment Selection. Am Soc Clin Oncol Educ Book. 2020 Mar;40:1-10. doi: 10.1200/EDBK_280775. PMID: 32213087. [4] Kushnarev V, Stupichev D, Kryukov K, et al143 Correlating RNA-seq detection and IHC staining of potential antibody-drug conjugate (ADC) targets: HER3, HER2, TROP2, Nectin4, and aFLRJournal for ImmunoTherapy of Cancer 2023;11:doi: 10.1136/jitc-2023-SITC2023.0143 [5] Ascione L, Crimini E, Trapani D, Marra A, Criscitiello C, Curigliano G. Predicting Response to Antibody Drug Conjugates: A Focus on Antigens' Targetability. Oncologist. 2023 Nov 2;28(11):944-960. doi: 10.1093/oncolo/oyad246. PMID: 37665782; PMCID: PMC10628585. [6] Paolo F. Caimi, Mehdi Hamadani, Carmelo Carlo-Stella, Masoud Nickaeen, Eric Jordie, Kiersten Utsey, Tim Knab, Francesca Zammarchi, Serafino Pantano, Karin Havenith, Ying Wang, Joseph Boni; CD19 Expression by IHC Alone Is Not a Predictor of Response to Loncastuximab Tesirine: Results from the LOTIS-2 Clinical Trial and Quantitative Systems Pharmacology Modeling. Blood 2022; 140 (Supplement 1): 9548–9550. doi: https://doi.org/10.1182/blood-2022-159626
Advancements in bispecific antibody research and innovative platforms
Bispecific antibodies represent a groundbreaking innovation in cancer immunotherapy. By binding to two distinct antigens simultaneously, these molecules direct immune cells to target cancer cells with precision, enhancing immune-mediated killing. The development of these therapies has opened new frontiers in oncology, with preclinical platforms playing a pivotal role in evaluating their efficacy, safety, and mechanisms of action before clinical trials. History and Challenges of Bispecific Antibodies Research The concept of bispecific antibodies originated in the 1960s, with the first experimental bispecific constructs developed in the 1980s using chemical cross-linking. Early versions were limited by instability and production challenges. Advances in genetic engineering in the 1990s led to the creation of more stable and functional bispecific molecules. Over time, the field has evolved to include trispecific, tetraspecific, and even pentaspecific antibodies, each designed to address specific therapeutic needs by engaging multiple targets or pathways simultaneously. The structural complexity of these molecules has grown, incorporating modular designs like dual-variable domain antibodies and Fc-engineered formats to enhance therapeutic efficacy and half-life. [1, 2] The dual mechanisms of bispecific antibodies pose unique challenges in preclinical research. Traditional cell line-based models often fail to replicate the intricate interactions within the tumor microenvironment (TME), limiting their predictive power. Advanced models that closely mimic human tumor biology are required to fully understand the therapeutic potential and risks of bispecific antibodies. Testing Bispecific Antibodies: In Vivo and Ex Vivo Approaches Advanced preclinical models have been used to evaluate the performance of bispecific antibodies. Among the pre-clinical models, patient-derived xenografts (PDX) are invaluable for maintaining the genetic and histological fidelity of patient tumors. Representing the testing platform closer to the clinic, these models allow researchers to study tumor-specific responses and resistance mechanisms in vivo. Syngeneic models, using murine tumors in immunocompetent mice, provide insights into the immune system’s role in therapy efficacy. Yet, murine tumors and immune responses are very different from their human counterpart. While syngeneic models are a good proof of concept, they do not provide clinically translatable reliable data sets. [3] Humanized mice incorporating human tumors together with human immune cells are very important in the field. The standard models used to test bispecific are adoptive transfer models leveraging peripheral blood mononuclear cells (PBMCs) or CD34+ stem cells. These systems replicate the interactions within the TME, enabling the study of immune cell recruitment, activation, and cytotoxicity driven by bispecific antibodies. The integration of humanized mouse models, engrafted with PBMCs or CD34+ stem cells, enhances the translational relevance of these studies by mimicking human immune responses more accurately. The use of humanized mice models can be challenging; however, the right expertise can help the selection of the best strategy for each bispecific MoA or combinatorial treatment of interest with CPI. [4] Organoid models offer a controlled ex vivo environment to study complex cellular interactions, preserving the molecular diversity and histological characteristics of original patient tumors. Adding immune cells to organoids generating a co-culture assay enables researchers to analyze interactions between cancer cells and immune cells within a reconstructed TME. These assays provide critical insights into immune cell recruitment and cytotoxicity, key to understanding bispecific antibody mechanisms of action. Co-culture systems offer a high-throughput, controlled environment for testing bispecific antibodies, maintaining tumor heterogeneity and complexity, making them ideal for pre-clinical interrogation of different strategies to address the complexities of bispecific antibody research. In the hematologic malignancies field, leveraging primary, never-passaged, well-characterized patient material allows the evaluation of bispecific antibody efficacy in a clinically relevant ex vivo system where immune cell viability and function are retained. Conclusion The complexity of bispecific antibody mechanisms needs advanced preclinical platforms that accurately replicate human tumor biology, such as PDX in humanized in vivo hosts, organoids-based co-culture assays, and hematological platforms supporting immune cells, offering unparalleled tools for translational research. By integrating these platforms into bispecific antibody development, researchers can gain deeper insight into mechanisms of action, better predict therapeutic outcomes, and ultimately enhance clinical success. The future of bispecific, trispecific, and even pentaspecific antibody therapies and the combination with checkpoint inhibitors hinges on the optimal selection and execution of specific translational strategies leveraging these innovative preclinical models.
Advances in BCMA-Targeting Therapies: Takeaways from ASH2024
This year’s ASH conference saw a significant focus on multiple myeloma. Arcellx's Gilead-partnered CAR-T therapy, anitocabtagene autoleucel was a major highlight. At a follow-up of 34 months, a single anito-cel infusion delivered early, deep, and long-lasting responses in patients with heavily pretreated relapsed or refractory multiple myeloma (RRMM). Remarkably, the complete response rate reached 79%. Importantly, the treatment demonstrated a manageable safety profile.[1, 2] However, notable advancements in BCMA-directed multiple myeloma therapies extend beyond CAR-T, with a focus on antibody formats. An interesting update concerned ABBV-383, a T-cell engager developed by AbbVie following its acquisition of TeneoOne. Recent data highlight promising outcomes for ABBV-383 in combination with Darzalex and dexamethasone, yielding an overall response rate (ORR) of 70%, which rises to 82% at higher doses. This development builds on AbbVie's earlier report of a 57% ORR from ABBV-383 monotherapy trials and underscores AbbVie's commitment to this area.[3, 4, 5] Initial findings on EMB-06, a T-cell engager developed by EpiMab and subsequently licensed to Vignette Bio, were also presented [6]. Complementing these discussions of BCMA-targeted therapies, ASH also showcased updates on Bristol Myers Squibb's pipeline. This includes its immunomodulatory cereblon E3 ligase modulators (celmods), such as mezigdomide, golcadomide, and iberdomide, aimed at extending the legacy of its Celgene-derived multiple myeloma treatments. [7, 8, 9, 10, 11] Beyond BCMA, BMS's anti-GPRC5D CAR-T candidate, BMS-986393, has demonstrated significant potential, with Phase 1 trials reporting an impressive 91% ORR among evaluable patients treated at the go-forward dose. These results have encouraged the initiation of the Phase 3 Quintessential-2 trial, scheduled to begin in early 2024. [12, 13] This year’s ASH also explored the management of precancerous conditions like smoldering myeloma, a primarily asymptomatic precursor to active multiple myeloma. Discussions focused on whether aggressive treatments, such as CAR-T therapy, are appropriate for managing these cases. The therapy's risks are highlighted by a study of Carvykti showing severe neutropenia in all patients and liver enzyme elevations in a subset [14]. Johnson & Johnson and Genmab’s Darzalex has shown promise in treating smoldering myeloma, with significantly improved progression-free survival compared to active monitoring (hazard ratio 0.49, p<0.0001) [15, 16]. Sanofi’s Sarclisa, also targeting this condition, is progressing through trials [17]. ASH 2024 delivered critical updates on these advanced clinical trials and therapies. The intersection of novel treatment modalities and evolving clinical strategies ensured the central role of this year's conference to the ongoing innovation in multiple myeloma and related indications. Champions Oncology offers a cohort of patient-derived primary multiple myeloma models for use in our ex vivo Hematological Vitroscreen. These extremely rare and well-annotated models can help advance your multiple myeloma research and accelerate your drug pipeline.
How to Develop Relevant Co-Culture Models of the Tumor Microenvironment
The Tumor Microenvironment: A Barrier to Effective Cancer Therapy The tumor microenvironment or TME is critical in shaping tumor progression, therapy resistance, and recurrence. The tumor microenvironment comprises stromal cells, immune cells, and signaling molecules that significantly impact how tumors respond to treatment. Immunosuppressive components of the tumor microenvironment, such as M2-polarized macrophages and activated cancer-associated fibroblasts (CAFs), foster resistance to therapies by creating an environment where immune responses are suppressed, and tumor survival is promoted. Key cytokines like IL-10 and TGF-β drive this immunosuppressive milieu, hindering the efficacy of immunotherapies and other anti-cancer treatments. Despite advancements, many cancer therapies fail in the clinical setting because the preclinical models used to evaluate them inadequately replicate the human tumor microenvironment. Addressing this issue is crucial for developing treatments that overcome tumor microenvironment-induced resistance and enhance clinical outcomes. The Limitations of Current Preclinical Models In Vivo Models: The Gold Standard, But Not Without Flaws In vivo models, particularly mouse models, have long been considered the gold standard for preclinical cancer research. However, they are not perfect, and it is important to know their limitations to navigate the field and select the right model for every application. While patient-derived xenografts (PDXs) maintain the genetic and histopathological features of human tumors and are considered an optimal model for clinical translatability of pre-clinical testing, the stromal compartment—including vasculature, immune cells, and fibroblasts—originates from the mouse host. This murine stroma fails to fully replicate the complexity and behavior of the human tumor microenvironment, limiting translational relevance. Humanized mouse models attempt to overcome some of these limitations by engrafting human immune cells into immunodeficient mice. While this approach provides valuable insights into immuno-oncology, it does not incorporate other critical human stromal components, such as CAFs and endothelial cells. This leaves a significant gap in accurately modeling the human tumor microenvironment, particularly when studying immunosuppressive mechanisms and therapy resistance. Simpler Models: Insufficient for Complex Therapeutic Mechanisms Monocultures of cancer cell lines, while failing to account for the intricate interactions between tumor cells and the surrounding tumor microenvironment, also lack tumor heterogeneity. The absence of stromal components in these models overlooks key factors influencing therapy mechanisms of action (MoA), particularly those targeting the tumor microenvironment. For example, therapies designed to modulate immune responses or disrupt fibroblast-mediated immune suppression are significantly affected by the presence and functionality of tumor microenvironment components. Consequently, these simplistic models often yield non-translatable results, leading to failure in clinical trials. The Tumor Microenvironment's Role in Resistance, Recurrence, and Progression The tumor microenvironment is a dynamic and interactive ecosystem that evolves with tumor progression. Specific elements of the tumor microenvironment, such as M2 macrophages and CAFs, actively promote resistance and recurrence by suppressing anti-tumor immunity and enhancing tumor survival. M2 Macrophages secrete IL-10, TGF-β, and VEGF, promoting immune evasion, angiogenesis, and tumor progression. CAFs can contribute to the desmoplastic reaction and produce extracellular matrix proteins, such as collagen, which act as physical barriers to therapy. They also release CXCL12 and TGF-β, further suppressing immune cell infiltration and activity. Therapies targeting these immunosuppressive mechanisms have shown promise in preclinical settings but often fail in clinical trials due to the lack of a human-relevant tumor microenvironment in the models used for their development. To address these challenges, advanced ex-vivo co-culture models that mimic the human tumor microenvironment are essential. These models integrate multiple human cellular components, including tumor cells, immune cells, fibroblasts, and endothelial cells, in ratios and conditions that closely resemble specific tumor types. Advantages of Ex Vivo Co-Culture Models By using human cells for all tumor microenvironment components, these models eliminate the cross-species differences inherent in mouse models. The proper characterization and ratios of human stromal cells enable accurate modeling of tumor microenvironment-driven mechanisms, such as immunosuppression and fibrosis. Real in-depth research is needed on the tumor microenvironment composition of different human tumors before starting to generate co-culture mimicking the tumor microenvironment. To provide better translational relevance, it is ideal to leverage Patient Derived Xenograft-organoids (PDX-O) a valuable source of tumor cells that retain the heterogeneity and genetic complexity of the original tumor providing data that more closely predict clinical outcomes, reducing the high failure rate of therapies in clinical trials. Ultimately, using PDX-Os combined with human stromal and immune components in co-culture models creates a system that mirrors the patient-specific tumor microenvironment, enabling the evaluation of therapies in a clinically relevant context. Applications of Ex Vivo Tumor Microenvironment Models: CAR-T Cell Therapy in Immunosuppressive Tumor Microenvironment CAR-T cell therapy, a breakthrough in cancer immunotherapy, often struggles in solid tumors due to the immunosuppressive TME. M2 macrophages and CAFs inhibit CAR-T cell infiltration and activity through the secretion of TGF-β and CXCL12. Recent studies have demonstrated that anti-TGF-β antibodies or CXCR4 inhibitors can restore CAR-T cell functionality in ex-vivo co-culture models, highlighting the importance of these models for optimizing CAR-T therapeutics targeting CAFs [1]. Similarly, antifibrotic agents, such as inhibitors of lysyl oxidase (LOX) or TGF-β signaling, aim to disrupt the fibrotic stroma created by CAFs. Using ex vivo tumor microenvironment models, researchers have shown that these agents enhance the penetration and efficacy of chemotherapies and immunotherapies [2]. This highlights the key role these models can play in evaluating combination strategies targeting both the tumor and its microenvironment. Developing Strategies to Mimic the Human Tumor Microenvironment Creating robust ex-vivo tumor microenvironment models requires careful selection and characterization of human cells. Strategies include the selection of the right tumor microenvironment cells from the right origin, using the best E:T ratio between immune cells and patient-derived tumor cells, and defining optimal ratios of immune cells, fibroblasts, and endothelial cells to replicate a model-specific tumor microenvironment. In addition, functional validation is fundamental in ensuring that all cellular components behave as they do in vivo, including cytokine secretion and immune cell polarization. These considerations are critical for generating data that can effectively guide clinical decision-making. Bridging the Gap to the Clinic The development of human-relevant ex vivo co-culture models represents a significant step forward in cancer research. By faithfully replicating the human tumor microenvironment, these models provide a powerful platform for studying therapy resistance, optimizing treatment strategies, and improving the clinical translatability of preclinical findings. Ultimately, this approach aligns with the goal of delivering better outcomes for cancer patients.
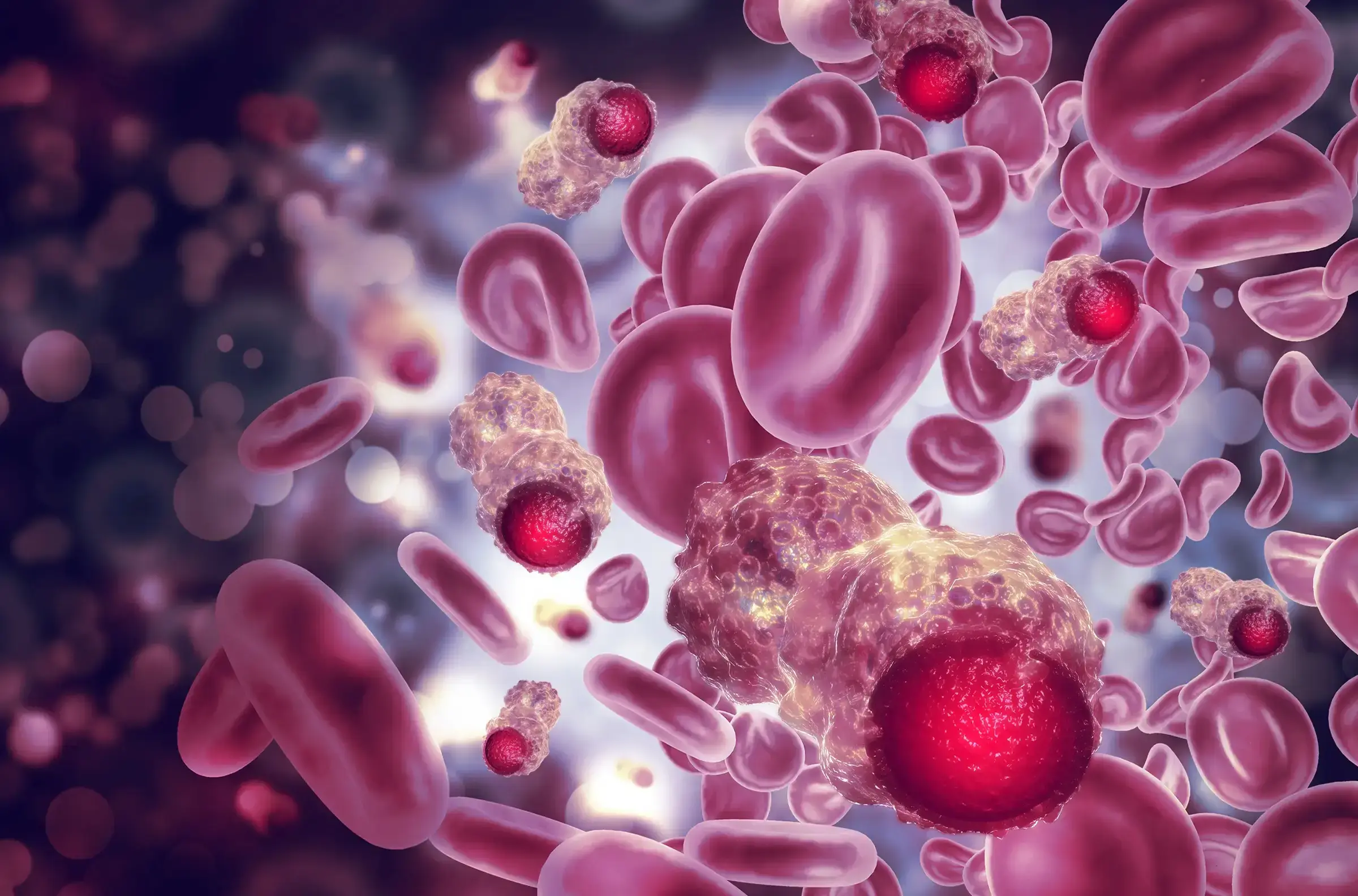
Bad Blood: Modeling Biologically Relevant Blood Cancer Studies
In the vast and intricate world of cancer research, blood cancers—such as leukemia, lymphoma, and myeloma—pose unique challenges. Unlike solid tumors, these malignancies originate in the bone marrow and affect the production and function of blood cells. For scientists, understanding these diseases is crucial for developing effective treatments and enhancing patient outcomes. The quest to understand blood cancer has driven scientists to develop innovative modeling techniques that mimic the disease's progression and response to treatments. Among these, ex vivo and in vivo models stand out as vital tools, each offering distinct insights and challenges. This blog post will explore the intricacies of these blood cancer modeling approaches, highlighting their advantages, limitations, and relevance in modern-day blood cancer research. Understanding Ex Vivo and In Vivo Modeling in Blood Cancer Studies To fully appreciate the nuances of blood cancer research, one must first grasp the fundamental differences between ex vivo and in vivo modeling. Ex vivo models refer to experimental setups where peripheral blood cells or bone marrow that contain the leukemic cells are taken from an organism and studied outside of their natural environment, in a controlled laboratory setting. This allows researchers to examine cellular behaviors and responses with precision, free from the complexities of a living organism. In contrast, in vivo models of blood cancer involve studying the disease within a living organism, typically using animal models like mice. This approach provides a more holistic view of how a disease behaves in a complex biological system, considering factors such as immune responses and interactions with other tissues. While both models are invaluable for blood cancer research, their applications and insights can vary significantly depending on the research question at hand. Advantages and Limitations of Ex Vivo Models The use of ex vivo models in blood cancer research is favored by the access to tumor cells from the blood. This approach allows for a direct detailed examination of cellular processes, enabling researchers to manipulate and observe how blood cancer cells react to specific treatments or conditions soon after they are extracted from the patient. This level of control is essential for understanding how certain therapies affect blood cancer cell survival and proliferation. As such, ex vivo models can provide rapid results and researchers can quickly gather data and adjust their experiments accordingly. This accelerates the pace of discovery and innovation in the blood cancer field. Primary Blood Cancer Models vs Immortalized Cell Lines One significant advantage of primary blood cancer models over cell lines is their ability to more accurately reflect the genetic and phenotypic diversity of actual patient tumors. Cell lines, although useful, undergo genetic drift and become less representative of the original tumor's complexity. In contrast, primary models of blood cancer, derived directly from patients' samples, retain the heterogeneity and specific characteristics of the patient's disease. This fidelity ensures more reliable insights into the tumor's behavior and response to therapies, which is crucial for developing personalized treatment strategies and improving clinical outcomes in blood cancer research. Co-Cultures in Primary Blood Cancer Models Co-cultures in primary blood cancer models provide an advanced method to closely simulate the tumor microenvironment by cultivating blood cancer cells alongside other relevant cell types, such as stromal or immune cells. This technique enriches the blood cancer model's complexity, shedding light on critical cellular interactions and signaling pathways that drive blood cancer progression and resistance to treatments. By incorporating multiple cell types, co-cultures facilitate exploration of the tumor cell clonality and dynamic interaction with the surrounding microenvironment by flow cytometry and/or high-content imaging within a more physiologically relevant context. Consequently, they enhance the accuracy of predictions related to therapeutic responses and enable the development of more targeted and effective treatment strategies for blood cancers. Limitations of Ex Vivo Models Ex vivo models of blood cancer are not without their limitations. The primary challenge lies in their inability to replicate the complex interactions that occur in a living organism. Factors such as immune responses, microenvironmental influences, and systemic effects are often absent in ex vivo setups, potentially leading to results that may not fully translate to in vivo scenarios. Advantages and Limitations of In Vivo Models In vivo models bring a different set of strengths to blood cancer research. Their greatest advantage is the ability to study blood cancer within the context of an entire living system. This provides insights into how blood cancer interacts with the host's immune system, how treatments affect overall health, and how the disease may evolve over time. Through in vivo blood cancer studies, researchers can observe the effects of a treatment on both the tumor and the host. This holistic view is crucial for understanding not only the efficacy of a therapy but also its potential side effects and long-term consequences. Despite these benefits, in vivo models of blood cancer have their own set of challenges. They can be time-consuming and costly, requiring significant resources to maintain and execute. Finally, there is always the risk that findings in animal models of blood cancer may not perfectly translate to human patients. Challenges of Modeling Blood Cancer In Vivo Patient-derived xenograft (PDX) models can be generated for some blood cancer indications. This approach involves implanting patient tumor cells into immunocompromised mice and passaging the tumor into a series of mice to establish a stable model. Although these blood cancer models are a better representation of the clinical disease compared to cell lines, due to passaging, PDX models from multiclonal blood cancer such as AML would not retain the cellular and molecular heterogeneity typical of the patient’s disease, limiting their clinical relevance. Instead, primary patient-derived models of blood cancer created by implanting patient tumor cells into immunocompromised mice for in vivo studies not only preserve the genetic characteristics of the original tumor but also, and most importantly, retain the heterogenic nature of the patient’s disease, therefore providing a closer representation of blood cancer like AML in patients. However, they can be difficult to develop and maintain, limiting their widespread use. The Importance of Diverse Modeling Approaches in Blood Cancer Research In the quest to cure blood cancer, no single modeling approach offers all the answers. Both ex vivo and in vivo models of blood cancer have their place in the research ecosystem, each contributing valuable insights to our understanding of these complex diseases. For scientists, the key lies in leveraging the strengths of each approach and exploring new technologies that bridge the gap between precision and biological relevance in blood cancer research. By doing so, we can continue to push the boundaries of what is possible in blood cancer research, ultimately improving the lives of patients worldwide. Champions Oncology has assembled a comprehensive collection of platforms encompassing a diversity of blood cancer types, including AML, B-ALL, T-ALL, CLL, DLBCL, MCL, MDS, and MM, directly from primary patient samples. This living bank of primary tumors empowers our clients to evaluate the efficacy of innovative therapeutic strategies with remarkable precision both in vivo and ex vivo. By encapsulating the intricate biology of blood cancer and mirroring the considerable heterogeneity inherent in patient populations, our platform is at the forefront of facilitating a rapid transition from bench to bedside.
Primary Blood Cancer Models: Getting Blood from a Stone
In the intricate maze of biomedical research, the quest for accuracy and relevance often leads to one pivotal question - which model systems offer the most reliable insights? The choice of a reliable system becomes even more mandatory for hematologic malignances, and in particular Acute Myeloid Leukemia (AML), that are inherently characterized by a high degree of heterogeneity. Among all the options, primary blood cancer models stand out as high-fidelity systems. These models, rooted in the direct application of human samples, are redefining how researchers approach complex biological questions. For those, scientists focused on pharmaceutical development in oncology, understanding the nuances of these models could unlock new pathways in their investigations. Why Primary Blood Cancer Models Are Gaining Ground The use of primary blood cancer models is critical for scientists to be able to mirror clinical outcomes, however, the field is still impacted by the access to only poor-quality models. Understanding why primary blood cancer models are increasingly preferred over cell lines and, in some cases, over traditional patient-derived xenograft (PDX) models is imperative. Specifically, for some hematological malignancies such as AML, it has been shown that there is an important loss of disease multiclonality at early passages [1]. Primary AML Models’ Edge Over PDX Models When it comes to AML, primary models offer several distinct advantages over serially passaged PDX models. First, they provide a closer genetic match to the human condition, enabling more precise interpretations of how tumors behave in vivo. Additionally, the primary models maintain the original AML heterogeneity, providing valuable insights into the mechanisms driving tumor progression and drug response. This fidelity is crucial for researchers aiming to unravel the complexities of AML biology. Unlike serially passaged AML PDX models, which can lose critical human-specific characteristics over time due to adaptation in a non-human host and undergo clonal selection through passaging, primary AML models maintain cellular integrity and relevance. A Step Towards Personalized Medicine By mirroring human physiological conditions more accurately, primary blood cancer models facilitate the development of personalized medicine. Researchers can test how individual patients might respond to specific treatments, paving the way for tailored therapeutic strategies. This approach may not only improve patient outcomes but also enhance the efficiency of clinical trials by identifying the most promising candidates early in the process. Biopharma Development on the Horizon For biopharma companies, primary heme models present opportunities for innovation. These models allow scientists to identify potential drug candidates more rapidly and with greater accuracy, minimizing the risk of late-stage clinical trial failures. By incorporating primary blood cancer models into the drug development pipeline, biopharma companies can streamline their processes, reduce costs, and ultimately bring life-saving therapies to market faster. A New Era for Translational Research Translational research aims to bridge the gap between laboratory findings and clinical applications. Primary blood cancer models serve as a catalyst in this process, enabling researchers to translate basic scientific discoveries into therapeutic interventions more efficiently. Their ability to mimic human physiology closely ensures that findings in the lab are more likely to be relevant to patient care, enhancing the overall impact of research efforts. Practical Tips for Incorporating Primary Blood Cancer Models While the benefits of primary blood cancer models are clear, integrating them into research methodologies requires careful planning and execution. Here are some practical tips for researchers looking to harness the power of these models. Building a Robust Infrastructure Establishing a successful primary blood cancer model system begins with creating a robust infrastructure. This includes acquiring high-quality primary human blood samples, ensuring proper storage and handling protocols, and investing in the necessary equipment and technology. Collaborative partnerships with hospitals and biobanks can facilitate access to diverse tissue samples, enhancing the diversity and applicability of the research. Working with an expert provider that has access to a deep clinical network can solve both the sample procuring and technical complexity issues. Champions Oncology offers the largest bank of engraftable primary blood cancer models. Our continued effort in sourcing the most clinically relevant tumors and our proved expertise in hematological tumor studies make us the best partner to help you advance your blood cancer pipeline. Addressing Common Challenges and Misconceptions Despite their potential, primary blood cancer models come with their own set of challenges and misconceptions. It is crucial for researchers to be aware of these and adopt strategies to overcome them. Overcoming Technical Limitations One common challenge is the technical complexity involved in establishing and maintaining primary blood cancer models. Researchers must be diligent in optimizing culture conditions, monitoring cell viability, and ensuring the reproducibility of results. Regular quality checks and standardization of protocols can mitigate these challenges and improve the reliability of the models. Researchers should also remain open to exploring new technologies and methodologies that can enhance the performance of primary blood cancer models. Continuous innovation and adaptation are essential to address evolving research needs and maximize the potential of these models. Debunking Misconceptions There are several misconceptions surrounding the use of primary blood cancer models, particularly regarding their cost and scalability. While initial investments may be required, the long-term benefits of these models often outweigh the costs. Their ability to provide more accurate and relevant insights can lead to more successful research outcomes and, ultimately, cost savings. Another misconception is that primary blood cancer models are only suitable for specific research areas. In reality, their versatility makes them applicable across a wide range of biomedical fields, from cancer research to regenerative medicine. Researchers should explore the diverse applications of these models and consider incorporating them into their own research endeavors. In conclusion, primary blood cancer models represent a significant step forward in biomedical research. Their ability to provide accurate, relevant insights makes them an invaluable tool for researchers across a wide range of fields. By adopting these models, researchers can enhance their research outcomes, drive innovation, and ultimately improve patient care.
It’s All in the Blood: Choosing Clinically Relevant Blood Cancer Models for Research
Acute Myeloid Leukemia (AML) presents a remarkable challenge in oncology, characterized by the rapid growth of abnormal white blood cells. Developing clinically relevant research models is crucial for scientists to understand and treat AML effectively. These models can simulate the disease's complexity, providing insights into its progression and aiding in the development of targeted therapies. The Importance of Heterogeneity in AML One of the most significant hurdles in AML research is its heterogeneity. AML is not a homogeneous disease but a collection of diverse subtypes, each with its own genetic and molecular characteristics. Each patient's tumor is composed of several different malignant myeloid blast cell subpopulations that make each tumor unique. This diversity impacts clinical outcomes and treatment responses, making it essential for researchers to use models that accurately reflect this heterogeneity. By acknowledging and incorporating this variability, researchers can better predict patient responses to new treatments. (Read our blog "A Needle in a Haystack: Finding Rare AML Populations by Flow Cytometry") Exploring AML Model Options There are several AML models available, each offering unique insights and benefits: Cell Line Models Cell line models are often the first step in AML research. These models allow researchers to study specific cellular processes in a controlled environment. However, they do not capture the complexity of the disease due to their homogeneous nature. Despite this limitation, cell lines can be useful for initial screenings and mechanistic studies. Patient-derived xenografts (PDX) PDX models involve implanting patient tumor cells into immunocompromised mice and passaging the tumor into a series of mice to establish a stable model. Although these models are a better representation of the clinical disease compared to cell lines, due to passaging, PDX models do not retain the cellular and molecular heterogeneity typical of AML, limiting their clinical relevance. Primary patient-derived models Primary patient-derived models are created by culturing primary AML cells from patient samples for ex vivo use or implanting patient tumor cells into immunocompromised mice for in vivo studies. These models not only preserve the genetic characteristics of the original tumor but also, most importantly, retain the heterogenic nature of the patient’s disease, therefore providing a closer representation of AML in patients. This approach also preserves the tumor's microenvironment, allowing researchers to study how it interacts with treatments. However, they can be difficult to develop and maintain, limiting their widespread use. (Learn about our ex vivo hematological model offering) Champions’ Medical Affair team continuously procures primary AML samples representative of the heterogeneity of the patient population, and our expert team develops and validates their growth in our experimental settings. We offer a large bank of primary, never passaged, AML models for ex vivo and in vivo use. Our oncology experts can help you achieve your research objectives from model selection and study planning to data analysis and result interpretation. (Explore our in vivo hematological model offering) Selecting the Right Type of AML Model Choosing the appropriate AML model depends on the specific research objectives. Researchers should as always try to match the research question with the complexity of the model, and the available resources. For instance, cell line models may suffice for preliminary studies, while patient-derived models are preferable for testing targeted therapies. Collaborations with experienced organizations, like Champions Oncology, can provide valuable insights and access to tailored experimental solutions. (Contact us) The Role of Clinical Annotations Incorporating clinical annotations into AML model characterization is crucial to select the right models for replicating patient scenarios accurately. Champions primary AML models are deeply characterized and extensively annotated. These annotations provide context, linking laboratory findings to real-world patient data. By integrating molecular characteristics with clinical information such as treatment history and patient outcome, researchers can enhance the relevance and predictive power of the results obtained. This approach bridges the gap between experimental research and clinical application. (Dive into Lumin, our extensive multi-omics and multimodal database at lumin.bio) The ongoing evolution of models and technologies promises a brighter future for AML research, ultimately bringing us closer to effective treatments and cures. The choice of clinically relevant AML models is vital for advancing oncology research in this field. By recapitulating the disease heterogeneity and incorporating clinical annotations, Champions’ AML models from primary patient samples help researchers drive meaningful discoveries that will eventually improve patient outcomes. By leveraging the expertise of leading organizations like Champions Oncology, you can access the tools and insights needed to elevate your research and make a lasting impact in the fight against AML.
PDX Models: Masters of Diversity
Cancer research is constantly evolving, seeking new methods to better understand and treat this complex disease. Among the most groundbreaking developments in this field are patient-derived xenograft (PDX) models. These models have revolutionized our approach to studying tumors by preserving the heterogeneity and molecular characteristics of a patient's tumor. This blog post aims to provide an in-depth look at the heterogeneity of PDX models and why it’s important to have diversity in your preclinical in vivo studies. The Importance of PDX Models Unlike traditional cell line-based models, PDX models retain the genetic diversity and molecular complexity of the original tumor. PDX models offer researchers a closer approximation of how human tumors behave in vivo, with different cell populations responding differently to therapies. They provide a dynamic and clinically relevant platform for studying tumor growth, metastasis, and response to treatment, making them a powerful tool in the fight against cancer. (Read our blog "The Ultimate Guide to Designing a Mouse Clinical Trial and Data Analysis") Models pretreated with targeted therapies are ideal to test next-generation agents. For example, when developing a drug that aims to overcome resistance to the standard of care therapy in a given tumor type, choosing models pretreated with that standard of care agent for our efficacy study will reveal true therapeutic effects in the target patient population. (Read our blog "Accelerating Innovation & Drug Development with Pre-treated PDX Models") Tumor Heterogeneity of PDX models is important for translational oncology studies One of the most significant advantages of PDX models is their ability to preserve tumor heterogeneity. Tumors are not uniform; they consist of various cell types with different genetic mutations and behaviors. On the contrary, traditional cell lines are developed in vitro by clonal selection, leading to a less accurate representation of the human disease.[1] PDX models also retain the molecular characteristics of the original tumor. This includes genetic mutations, epigenetic modifications, and gene expression patterns. By maintaining these features, PDX models provide a more accurate representation of the human tumor genetic background, which is crucial for developing effective therapies.[1] Advancing Cancer Research with PDX Models The ability of PDX models to preserve tumor heterogeneity and molecular characteristics has significantly advanced cancer research. Researchers can study the behavior of different tumor subpopulations, identify potential targets for therapy, and evaluate the efficacy of new treatments in a more realistic setting. PDX models have heterogeneous biomarker expression. The figure below, for example, shows the expression of KRAS in Champions’ PDX models varying across and within tumor types. Selecting PDX models with a higher KRAS expression will be paramount to successfully test KRAS inhibitors and could provide more clinically relevant results. Nonetheless, a PDX model with elevated KRAS expression will still present with heterogeneous expression across the different cell clones within the tumor, a setting that realistically reproduces the human tumor heterogeneous cell composition. In this setting, a KRAS inhibitor might only be partially effective at killing the tumor because cell clones with lower KRAS expression within the tumor might not be affected, resulting in lower overall therapeutic efficacy. Similarly, in the clinic, we could observe a partial response followed by tumor progression, due to the selection of the low KRAS-expressing cell clone within the tumor. For this reason, studies that use PDX models instead of cell line-derived models will produce more reliable and clinically relevant results. KRAS gene expression across Champions' PDX models of different tumor types. Patient-derived xenograft models have revolutionized cancer research by providing a more accurate representation of human tumors. Their ability to preserve tumor heterogeneity and molecular characteristics makes them an invaluable tool for studying cancer biology, testing new therapies, and personalizing treatment plans. By continuing to develop and refine these PDX models, researchers can accelerate the discovery of new treatments and bring them to patients faster. Champions Oncology has over 1500 clinically relevant PDX models that can accelerate your oncology research program. Our models have broad clinical annotation and have been deeply characterized using NGS (WES & RNA-seq), proteomic, and phospho-proteomic datasets to interrogate the heterogeneity of the tumor. To learn more about our PDX tumor models, access Lumin Analytics.
