Trends in Oncology
Harnessing the Power of Oncolytic Viruses in the Fight Against Cancer
We typically consider viruses as infectious agents or vaccine vectors, which are non-replicating entities that express vaccine antigens. More recently, researchers have been working to develop oncolytic viruses, which are engineered to specifically infect and replicate in tumor cells. This targeted infection results in tumor cell lysis, activation of anti-tumor immune responses, and the release of new oncolytic virus particles that can infect other tumor cells. The concept of oncolytic viruses emerged in the early 20th century when scientists observed that a leukemia patient spontaneously went into remission for a brief time following an influenza virus infection. Early attempts to develop non-specific oncolytic viruses were plagued with complications related to poor efficacy and safety issues. As our understanding of targeted immunotherapy for the treatment of tumors has evolved, oncolytic viruses are gaining traction again and an oncolytic herpesvirus (talimogene laherparepvec or T-VEC) engineered to target metastatic melanoma was approved for clinical use by the FDA in 2015 [1]. Advantages of Oncolytic Viruses Oncolytic virus development has expanded significantly in the last two decades. Some of the most widely used viruses that are engineered to target tumors include adenoviruses, alphaviruses, herpes simplex viruses (HSV), rhabdoviruses, and vaccinia viruses. Viruses can be engineered to target tumor cells for lysis, such as replication-competent HSV-1 deletion mutants (e.g. thymidine kinase or ribonucleotide reductase mutants) that can only replicate in rapidly dividing tumor cells. Similarly, T-VEC is a modified HSV-1 virus with a gene deletion in ICP34.5, which allows for antiviral responses by normal cells but not tumor cells, thus allowing for tumor-specific virus-mediated destruction [2]. Oncolytic viruses can be modified to express immune molecules (e.g. TNF, IL-12, or chemokines) that promote proinflammatory responses and increase recruitment of macrophages and T cells for enhanced antitumor immunity in addition to oncolytic activity [3-4]. Oncolytic viruses can also induce apoptosis of tumor cells or enhance the uptake of chemotherapeutic agents [5]. Currently under pre-clinical investigation is a vaccinia virus carrying a TGFβRII inhibitor that has proved effective in causing tumor regression in mouse tumor models and shown an even greater effect when combined with checkpoint inhibitor therapy [6]. This approach overcomes the difficulties of targeting TGFβ, limiting side effects due to the targeting of non-tumor cells. Another promising approach currently being evaluated pre-clinically is a therapy using CAR-T and TCR-T cells infected with myxoma virus. This approach induces autosis and adaptive immunity in mouse models of tumors to restrain antigen escape [7]. Some oncolytic viruses can induce long-term immunity to tumors and prevent metastasis or the re-occurrence of these cancers, thus making them attractive therapeutic candidates. Clinical trials using oncolytic viruses are currently ongoing for numerous solid tumor types including glioblastoma, breast cancer, lung cancer, and bladder cancer [8]. Evaluating Oncolytic Viruses Oncolytic viruses are typically grown in tissue culture systems and are evaluated in vitro using a panel of tumor cell lines, which provides insight into tumor specificity and mode of action. These modified viruses can then be tested in a wide range of animal models, including immunocompetent mice, such as those used for syngeneic mouse tumor models, and immunocompromised mice, which include humanized mice that carry patient-derived tumor xenografts. Certain oncolytic viruses, such as vaccinia virus, require that researchers be vaccinated against this virus before laboratory handling, but in most cases, these viruses can be handled under BSL-2 conditions. Conclusions Despite great success in preclinical studies, translating oncolytic virus therapy to the clinic can be quite challenging. One major obstacle is the route of administration, with the oncolytic viruses needing to be injected directly into the tumor. While this can be simpler for superficial tumors like melanoma, it becomes much more complex to reach tumors that grow in deeper body organs. Many different varieties of oncolytic viruses are currently being evaluated preclinically or in clinical trials and the next decade promises further advances in this cutting-edge field.
Ultimate Guide: Designing a Mouse Clinical Trial & Data Analysis
Cancer is a complex disease, and developing novel, effective treatments requires testing in preclinical models. Mouse clinical trials represent a critical step in translating promising anti-cancer therapies from bench to bedside. When combined with advanced bioinformatics and analytics tools, mouse clinical trials are a powerful experimental approach to identifying target patient populations, planning cohort extensions, selecting the right combination drug, elucidating the mechanism of resistance, or identifying translational biomarkers [1]. However, conducting a successful mouse clinical trial requires expertise in designing the study, analyzing the data, and interpreting the results. In this blog post, we will guide you through the essential steps of designing a mouse clinical trial and analyzing the resulting data. This guide includes tips on powering the study, preparing the dataset, grouping responders vs non-responders, identifying biomarkers, and integrating proteomics in a multiomics model. Step 1: Powering the study In a mouse clinical trial, animals implanted with PDX models are surrogates of the patients whom PDX models were derived from. Before starting a mouse clinical trial, it is essential to determine the sample size required to achieve reliable and statistically significant results. It is important to enroll a large enough number of PDX models (which corresponds to the number of patients we would enroll) and enough animals per PDX model (so as not to lose a patient if we lose a mouse). Power analysis will estimate the minimum number of animals needed to detect a difference in tumor growth inhibition (TGI) between the treatment and control groups. Typically, researchers set the power at 80% and α at 0.05, which means that there is an 80% probability of detecting a significant difference between the two groups if one exists. It is also recommended to power mouse clinical trials according to the study goal and endpoint. For instance, a survival endpoint may require larger group sizes than a TGI endpoint. If the goal of the mouse clinical trial is to identify a novel biomarker of response, a larger number of models will need to be included in the design. Step 2: Select models Model selection is a crucial step when designing a mouse clinical trial and needs to be done by taking into account several parameters associated with the clinical history and molecular characteristics of the models so that the PDX model panel recapitulates the targeted patient population. Tumor indication and/or mechanism of action of the drug are usually the two key parameters that guide PDX model enrollment in a mouse clinical trial, and the deeper the information in terms of clinical classification and molecular profiling the more representative will be the PDX model panel [2]. (Read our blog: "How to Use Metadata as Your Model Selection GPS") Step 3: Preparing the dataset Once the study is completed, the next step is to prepare the dataset for analysis. This includes checking for outliers and removing/excluding missing data. One critical factor in analyzing mouse clinical trial data is the identification of PDX models with common response profiles. This is usually evaluated by a modified version of the clinical Response Evaluation Criteria in Solid Tumors (mRECIST). The response rate can be calculated by comparing the tumor volume at day 0 either with the volume corresponding to the best response measured on treatment or with the tumor volume measured on the final day of treatment. The threshold value can vary depending on the tumor type and drug mechanism of action. Therefore, it is crucial to validate the threshold on a panel of known drugs. Step 4: Grouping responders vs non-responders Once the threshold is established, the next step is grouping responders vs non-responders. Responders are mice that show a reduction in tumor volume or mass greater than or equal to the critical value, and non-responders are mice that show tumor reduction below the critical value. These groups are used to compare gene expression profiles and identify potential biomarkers of response [3]. Step 5: Identifying biomarkers Bioinformatics analysis can be used to identify biomarkers of response. One widely used approach is differential gene expression analysis (DGEA), which compares the gene expression profiles of responders and non-responders to identify genes that are differentially expressed. Another approach is differential gene set enrichment analysis (DGSE), which identifies functional gene sets that are enriched in the responders and non-responders. Partial least-squares (PLS) regression, a dimensional reduction method part of DIABLO multi-omics integration workflow [4], is commonly used to identify the most influential genes within a multi-omics gene network that can predict response. It is very important that mouse clinical trials are designed accordingly when performing multi-omics analysis as an endpoint. (Watch our webinar: "Identify MOA and Companion Biomarkers in Oncology using Multi-Omic Analyses") Step 6: Integrating proteomics for improved target validation and biomarker identification Proteomics approaches, such as mass spectrometry-based proteomics, can provide quantitative information on protein expression levels and post-translational modifications. Given the lack of correlation between protein abundance and RNA expression, integration of proteomics and phospho-proteomics data in a multi-omics model can greatly improve the accuracy of therapeutic target expression for model selection, provide a more comprehensive understanding of the molecular mechanisms underlying drug response, and provide an important additional molecular annotation for biomarker identification via single or multi-omics analysis [5]. (Read our blog: "4D Proteomics: Adding Dimension to Protein Detection") In this blog post, we have provided a step-by-step guide on how to design and analyze a mouse clinical trial, and shown how a successful mouse clinical trial requires careful planning and expertise in bioinformatics. Lumin Acuity offers tailored bioinformatics and computational biology solutions to support your mouse clinical trial planning and data analysis, accelerating decision-making and driving actionable results. Well-designed and executed mouse clinical trials can be instrumental in developing effective cancer therapies and improving patient outcomes.
Advancing Therapeutic Strategies for Myelodysplastic Syndrome
Myelodysplastic syndromes (MDS) are a group of hematological malignancies that manifest in hematopoietic stem cells and are caused by ineffective hematopoiesis.[1] Currently, MDS is defined as unexplained cytopenia combined with abnormalities in cell maturation leading to dysplastic features in >20% of myeloid cells.[2] MDS is one of the most frequently diagnosed malignancies in the United States and progresses to acute myeloid leukemia (AML) in 30% of patients.[2] While the initiation of primary MDS is not well understood, research suggests that somatic DNA injury, defective DNA repair, impaired immunological responses, and dysfunctional cell signaling play an important role in early stage MDS development.[3] Like other malignancies, MDS is positively selected for through gene mutations[4] with the average MDS patient carrying nine somatic mutations, such as TET2, TP53, and RUNX1.[4, 5] These mutations may not directly drive MDS, however, evidence indicates that mutations to genes involved with DNA methylation and RNA splicing greatly contribute to dysregulation of genes critical to hematopoiesis, such as GATA1, KLF1, and HOXA9.[6] MDS is classically characterized as hematopoietic stem cells (HSC) with clonal advantages due to somatic mutations or cellular dysfunction, discussed above. Studies have also identified the critical role of bone marrow microenvironments (BME) in MDS progression, particularly cytokine alterations and activities. Across several studies, high serum levels of TNF-α, TGF-β, IL-6, and IL-8[7] are present in MDS patient bone marrow (BM).[8] These proinflammatory molecules are typically associated with higher apoptotic rates, and in MDS patients, molecules such as TNF- α, correlate to poor MDS treatment performance.[7] Furthermore, studies have also identified the critical role of malignant clones in MDS pathogenesis. Mesenchymal stromal cells (MSCs) are a key component of the bone marrow that regulate hematopoiesis and have immunomodulatory properties. In contrast, dysplastic MSCs in the bone marrow can create a microenvironment that supports clonal expansion of malignant cells. Dysplastic MSCs from MDS or AML patients have phenotypic abnormalities, including aberration in secreted proteins and cell surface protein expression, as well as increased senescence and decreased survival.[9,10] Disrupted methylation profiles are observed in both MDS malignant clones and MDS-MSCs. These methylation changes impact multiple signaling pathways which create a chronically inflamed BME that is harmful to normal HSCs and supports the expansion of MDS clones.[11] While less understood, de novo MDS has been linked to chemotherapy, radiotherapy, and environmental carcinogens like benzene.[12] Therapy-related MDS (tMDS) is prevalent in 10-20% of patients 20 years after chemotherapy and/or radiation, and the World Health Organization (WHO) recognizes alkylating agents, like topoisomerase II inhibitors, as initiators of tMDS.[12] Due to the high incidence of MDS in elderly populations[13] with co-morbidities, treatment by bone marrow transplantation is often contraindicated and few therapeutic options exist. Patients with MDS are typically divided into two different categories: low-risk MDS and high-risk MDS. The division of MDS into these two groups is useful for researchers and clinicians developing therapies for this highly heterogeneic disease.[14] Low-risk MDS therapies target symptoms of cytopenia through the use of erythropoiesis stimulating agents (ESA), such as epoetin alfa and darbepoetin alfa.[15] The Food and Drug Administration (FDA) has also approved two hypomethylating agents (HMAs), 5-azacitidine and decitabine, for use in patients with low-risk and high-risk MDS. While both standards of care noncompetitively inhibit DNA methyltransferase (DNMT1) and promote hypomethylation of DNA to block DNA synthesis,[16] 5-azacitidine integrates with RNA and interferes with ribosomal assembly to also limit tumor protein synthesis.[16, 17] In 2023, the FDA and European Medicines Agency (EMA) also approved luspatercept, a recombinant fusion protein that enhances late-stage erythroblast differentiation, for low-risk MDS. Luspatercept indirectly moderates ineffective erythropoiesis by interacting with broad spectrum inhibitory signals, namely transforming growth factor-β (TGF- β) superfamily signaling.[18, 19] Downstream, signaling molecules, SMAD2 and SMAD3, negatively regulate TGF- β. Luspatercept works by binding to activin receptor type IIB on TGF- β which disrupts SMAD2 and SMAD3 signaling therefore improving erythropoiesis and boosting RBC production in MDS patients.[20, 21] As our understanding of MDS pathophysiology improves, more effective treatment options will become available. Researchers are actively evaluating the toxicity of allogeneic hematopoietic stem cell transplantation, a therapy with curative potential.[19] Given the nature of such treatment which involves conditioning chemotherapy, the risk of aplasia and other graft-versus-host disease need to be adequately assessed. Additional studies, such as a newly announced Montefiore Einstein Comprehensive Cancer Center clinical trial,[22] are investigating new therapies to develop novel therapeutic strategies.
A Multi-Omics Driven Approach for Advancements in Pancreatic Cancer
Pancreatic ductal adenocarcinoma (PDAC) is one of the most common and aggressive forms of pancreatic cancer that has remained difficult to diagnose early and treat successfully. PDAC has a five-year survival rate below 10% and is one of the leading causes of cancer death. Complete surgical resection is one of the few curative treatment modalities, and chemotherapy protocols have limited efficacy[1]. Unfortunately, most existing immunotherapy-based treatments are also associated with poor response rates[2]. Recent analyses of PDAC samples have provided critical insights into genetic alterations that drive tumorigenesis and have identified potential therapeutic targets. Here we highlight several of these key findings and how they may lead to advances in PDAC treatment. PDAC arises in the epithelial cells of pancreatic duct, or ductules, and is thought to progress in a manner like other carcinomas, in which the normal epithelial cells transition into pre-invasive pancreatic intraepithelial neoplasia lesions that eventually form invasive PDAC[3]. Most PDAC tumors carry somatic mutations in oncogenes, particularly KRAS, TP53, CDKN2A, and SMAD4[4]. KRAS mutation is the most frequent event in PDAC. The assumption that KRAS is an undruggable target based on extensive drug screens that showed in vitro inhibition but limited or no efficacy in animal models[5] is finally being challenged by the very promising results obtained by administration of Sotoresib (KRAS p.G12C inhibitor) in patients with advanced pancreatic cancer (NCT03600883), and by the identification of small-molecules that inhibit KRAS p.G12D in preclinical studies[6,7]. The need for druggable targets or biomarkers for PDAC has led to more innovative approaches to identify unique molecule attributes. A recent comprehensive proteogenomic characterization of PDAC pancreatic ductal tissues compared against paired normal adjacent tissue, and the findings validated known mutations in oncogenes[8]. This study also defined previously unknown genomic alterations and analyzed differences in protein expression and protein phosphorylation status between tissues. This comprehensive analysis identified a panel of proteins linked to early stage PDAC, and phosphoproteomic analysis identified several signaling pathways downstream of KRAS, including PI3K/AKT/mTOR and MAPK/ERK, that may be targeted by existing kinase inhibitors. The PAK1/PAK2 kinases were also identified as dysregulated in PDAC tissues and have the potential to be targeted therapeutically. Recent studies have also better characterized the tumor microenvironment (TME) of PDAC and how this may limit treatment efficacy[9]. PDAC tumors tend to be highly heterogenous with a dense stroma and disorganized blood vessels, which impair drug penetration. The TME is enriched for myeloid derived suppressor cells and regulatory T cells and displays a low mutational burden, thus making this a “cold” tumor immunophenotype that is resistant to existing immunotherapies. Current studies are examining immunotherapy or drug-based strategies to turn “cold” PDAC tumors into “hot” tumors that would be receptive to immune checkpoint blockade. Further advances in PDAC research will require similar extensive proteogenomic studies that better define dysregulated pathways that trigger early events in tumor formation and may function as early biomarkers for disease. The search for novel therapeutic targets or combinations of targets is also essential to improving the currently dismal array of treatment options for PDAC patients. Champions Oncology has 81 highly characterized Pancreatic Cancer Models available for preclinical studies, click below to learn more about how these models can propel your research.
4D Proteomics: Adding Dimension to Protein Detection
The field of oncology research has evolved significantly over the years, with new technologies constantly emerging to improve our understanding and treatment of cancer. One such technology is 4D proteomics, which utilizes four dimensions (retention time, mass, intensity, and ion mobility) to improve the detection of low-abundant peptides in complex biological samples. This powerful technique has proven to be particularly useful in personalized medicine and biomarker discovery for cancer research[1]. What is 4D Proteomics? Proteomics is the study of all proteins present in a given sample or organism. Traditional proteomic methods have typically focused on identifying and quantifying proteins in a sample based on their mass and abundance. However, this approach often falls short when it comes to detecting low-abundant peptides, limiting our ability to fully understand the complexity of biological systems. That's where 4D proteomics comes in. This technique adds an additional dimension (ion mobility) to the traditional three dimensions of mass, retention time, and intensity. Ion mobility measures the ability of a molecule to move through a buffer gas under an electric field, providing another valuable data point to improve peptide separation and identification[1]. The Benefits of 4D Proteomics in Oncology Research The use of 4D proteomics has greatly improved the sensitivity and specificity of peptide identification, making it particularly useful in oncology research where small changes in protein levels can have significant implications. The addition of ion mobility as a fourth dimension has also improved peptide separation and identification, making it easier to analyze complex samples such as blood or tissue from cancer patients. This is especially crucial in personalized medicine, where individualized treatments are tailored to a patient's specific cancer and its unique molecular characteristics[2]. Additionally, ion mobility helps differentiate each phosphopeptide isoform, accurately identifying the phosphorylation site on the peptide and quantitating each peptide form. This is critical for example in measuring certain kinases whose activity or substrate selectivity is controlled by phosphorylation at specific sites[3]. Conclusion In conclusion, the use of 4D proteomics has revolutionized the field of oncology research by improving our ability to detect low-abundant peptides and analyze complex samples. This technology has proven to be particularly valuable in personalized medicine and biomarker discovery for cancer research. As more studies continue to utilize 4D proteomics, we can expect further advancements in our fight against cancer.
Recent Developments in Targeted Therapy for Non-Small Cell Lung Cancer
Lung cancer is an aggressive malignancy that correspond to approximately 12% of newly diagnosed cases per year and that remains one of the leading causes of cancer-related deaths (21%)[1]. Non-small cell lung cancer (NSCLC) is the most common form of lung cancer and is typically diagnosed at advanced stages[2]. Extensive genomic studies of NSCLC have been essential to identifying mutations that drive oncogenesis and has been critical to the development of targeted therapies. Here we highlight progress in NSCLC treatment and identify areas of ongoing research. Chemotherapy For decades, chemotherapy was the primary treatment for NSCLC, and platinum-based chemotherapies are still used today in combination with radiotherapy and targeted therapies[3]. Platinum-based chemotherapies have been improved since their initial development in the late 20th century, and “platinum doublets” or “triplets”, which combine two or three different platinum-based cytotoxic compounds, have been shown to better target NSCLC and cause less toxicity[4]. Chemotherapy is still used as a first line treatment for advanced NSCLC, but overall effectiveness is limited when used alone. Advances in targeted therapies and immune checkpoint blockade have greatly enhanced the effectiveness of chemotherapy on overall survival and progression-free survival[5]. Targeted Therapies Genetic analysis of NSCLC tumors has led to the use of targeted therapies. Mutations in the epidermal growth factor receptor (EGFR) were identified as the most prevalent defect in NSCLC patients across genders, ethnic groups, and smoking status[6]. Several common mutations have been characterized, but numerous rare mutations have also been identified, and most of these mutations target the tyrosine kinase domain, which results in unchecked cellular proliferation due to engagement of downstream MAKP, PI3K, and STAT signaling pathways. First (gefitinib and erlotinib) and second (afatinib and dacomitinib) generation tyrosine kinase inhibitors (TKIs) have been approved by the FDA to treat EGFR-mutated NSCLC. Unfortunately, treatment resistance and disease recurrence occur at a very high rate, and these TKIs are also associated with significant toxicity and undesirable side effects that result in adjustments of treatment regimens[5]. Third generation TKIs (e.g. osimertinib) that target specific EGFR mutations associated with acquired resistance to first and second generation TKIs have been approved and have been very successful in treating EGFR-mutated NSCLC as a first or a second line treatment. Because resistance to third generation TKIs eventually also arises, fourth generation TKIs are currently under development or are being used in ongoing clinical trials. Many of these next generation inhibitors have been carefully designed to optimize target specificity and reduce adverse events frequency and severity[7]. Mutations in other genes have also been observed at low frequency in NSCLC, and several clinical trials are now evaluating targeted therapies with inhibitors that target these genes, including, ALK, MET, ROS1, and BRAF among others[7, 8]. Capmatinib, an inhibitor targeting METex14 mutation, and adagrasib and sorotasib, both targeting KRAS G12C mutation, have recently been granted approval for treatment of NSCLC tumors presenting with the corresponding mutation[9, 10, 11]. In addition to small molecule inhibitors, Antibody-Drug Conjugates (ADC), a class of anti-cancer therapy capable of transporting cytotoxic drugs directly to tumor cells, are currently developed against NSCLC antigenic targets[12]. Immunotherapy Immunotherapies that target the immune checkpoint molecules like Programmed Death (PD)-1 or its ligand PD-L1 have been shown to have therapeutic effects as second-line treatments in combination with chemotherapy[13] for patients lacking mutations that can be treated with approved targeted therapies. While several of these trials have shown improvements in overall survival, serious adverse events have also been elevated. In addition to immune checkpoint targeting, other immunotherapies are currently under development, and a bispecific antibody has been recently approved for the treatment of a subset of NSCLC patients[14]. Biomarkers The availability of oncogenic driver mutations and of immune checkpoint targeted therapies have revolutionized NSCLC treatment and require the concomitant development of diagnostic tools to stratify patients and maximize the efficacy of these therapeutic options [15]. Oncogenic mutations are usually good companion biomarkers to indicate a patient as eligible to receive the associated treatment, however, diagnostic strategies need to be implemented to monitor patient response and anticipate or detect acquired resistance as early as possible. Immune checkpoint proteins are also currently tested as biomarkers to stratify patient, as an example a PD-L1 diagnostic test has been recently approved by FDA as companion biomarker to identify patients who are candidates for adjuvant treatment with atezolizumab [16]. Conclusion Advances in NSCLC have shifted the median overall survival from 2-4 months in the 1960s to more than 2 years since advent chemotherapy combined with immunotherapy or targeted inhibitors in the 2010s. Our deeper understanding of mutations that drive NSCLC and our ever-expanding arsenal of targeted therapies or immune modulators will further improve survival and quality of life for NSCLC patients.
Potentials of BTK Therapies for Chronic Lymphocytic Leukemia
Chronic lymphocytic leukemia (CLL) is one of the most common forms of adult leukemia, and its chronic nature has made it a challenging blood cancer to completely cure. CLL affects B cells and is typically classified into two categories: little or no somatic hypermutation in the immunoglobulin heavy chain variable region (IGHV), called unmutated CLL, or high mutation levels in the IGHV gene, called mutated CLL.[1] Unmutated CLL is more aggressive than mutated CLL, and the presence of these abnormal IGHV sequences, a part of B cell receptors (BCR), leads to abnormal BCR signaling and the uncontrolled proliferation of leukemic cells. Bruton’s tyrosine kinase (BTK) is an essential enzyme downstream from the BCR and is responsible for propagating the signaling cascade initiated by BCR engagement with pathogen-associated antigens.[2] Notably, BTK has been shown to be constitutively active in CLL and drives both leukemic cell proliferation and lymph node homing.[3] As antigen binds to the BCR, multiple protein tyrosine kinases are activated via interactions with the cytoplasmic domain of the BCR, including Lyn and Syk, as well as translocation of BTK to the plasma membrane through interactions with phosphatidylinositol-3,4,5 (PIP3).[4] Lyn and Syk phosphorylate BTK to activate multiple non-receptor protein tyrosine kinase signaling pathways, including NF-κB, MAPK, and phospholipase C gamma (PLCγ). Under normal conditions, this pathway leads to controlled B cell proliferation and differentiation, however, this same pathway leads to uncontrolled B cell proliferation in malignancies, such as CLL. The role of BTK in CLL has drawn researchers to develop BTK inhibitors, such as ibrutinib - an FDA (Food and Drug Administration)[5] and EMA (European Medicines Agency)[6] - approved CLL treatment. Ibrutinib forms a covalent bond with a cysteine residue (C481) at BTK’s active site, and thus inhibits kinase activity, including autoactivation.[3] This kinase inhibition shuts down BCR signaling, reduces B cell proliferation, and promotes apoptosis of leukemic cells. Ibrutinib is effective as a standalone treatment for mutated and unmutated CLL and when combined with rituximab is an effective therapy for relapsed CLL.[1] In general, ibrutinib is well tolerated and shows continued efficacy during extended treatment periods.[7] While ibrutinib has been a clinical success, there are a subset of CLL patients who develop resistance to this therapeutic. This resistance has been mapped to a C481S mutation that prevents ibrutinib from covalently binding to BTK resulting in continuous BCR signaling within leukemic cells.[3] Next-generation, reversible BTK inhibitors, such as ARQ 531, are currently being developed for relapsed/refractory CLL. ARQ-531 is a non-selective BTK inhibitor that suppresses signaling in cells with C481S BTK and PLCγ mutations. ARQ-531 also has an additional inhibitory activity against ERK signaling.[8] Furthermore, the FDA has recently approved LOXO-305, a non-covalent, reversible BTK inhibitor. LOXO-305 inhibits signaling in cells with wild-type or C481S-mutated BTK.[9, 10] In contrast, acalabrutinib, a second-generation irreversible BTK inhibitor has also been approved by the FDA. Acalabrutinib has a shorter half-life, allowing for variable dosages, and has increased C481 specificity that enhances its BTK inhibitory effects. The biochemical properties of acalabrutinib make it a suitable option for patients with treatment naïve CLL.[11] In January 2023, the FDA and EMA approved an additional second-generation irreversible BTK inhibitor, zanubrutinib, for CLL.[12] Zanubrutinib’s design was guided by a structure-activity strategy to generate sustained BTK occupancy. Zanubrutinib exhibits reduced ITK and EGFR inhibition and has 4x longer half-life than acalabrutinib.[13] As such, it persists at high concentrations within the body making it available to re-inhibit newly synthesized BTK proteins, a unique difference from ibrutinib and acalabrutinib.[14] In a phase I/II study, all CLL patients treated with zanubrutinib had complete and sustained BTK occupancy in peripheral blood mononuclear cells and lymph nodes.[15] Zanubrutinib’s performance supports the hypothesis that increased BTK selectivity maximizes BTK inhibition and drug efficacy. Additionally, zanubrutinib’s enhanced BTK specificity reduces the incidence of off-target toxicities which may reduce side effects commonly associated with ibrutinib, such as cardiac events, subdural hematomas, and gastrointestinal bleeding.[10, 16, 17] This is particularly relevant to CLL as this class of BTK inhibitors are used by CLL patients indefinitely. BTK inhibitors have become an invaluable CLL treatment and will continue to improve and provide therapeutic benefits. Additional studies such as NCT03734016 are underway to evaluate the effects of zanubrutinib and BTK inhibitors with other targeted therapies, which may improve the efficacy and durability of these treatments.
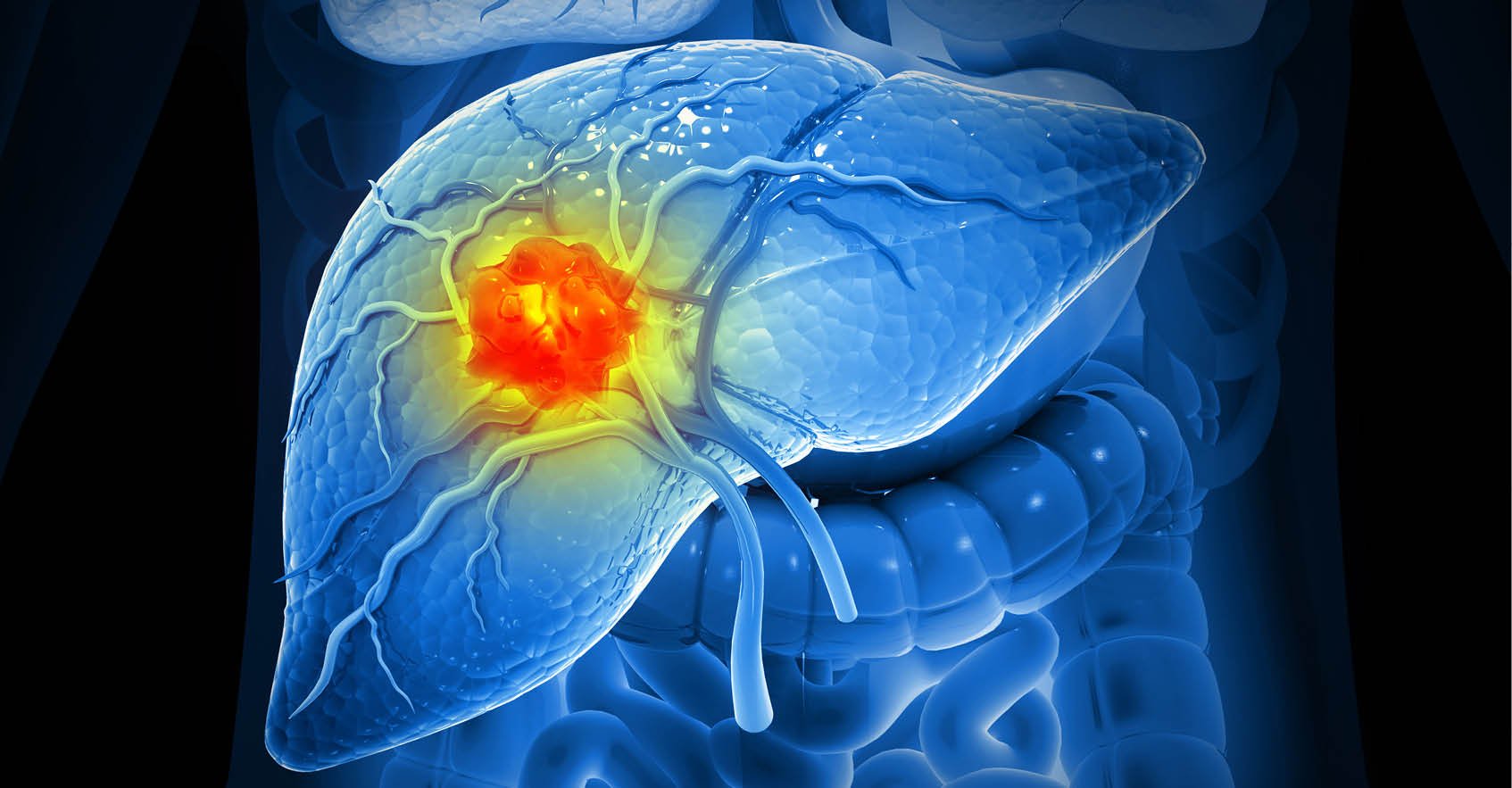
The Complex Case of Hepatocellular Carcinoma Clinical Management
Hepatocellular carcinoma (HCC) is one of the most prevalent types of liver cancer, and it usually develops in patients with underlying cirrhosis or chronic liver disease and metabolic syndrome.[1] HCC can spread to other body parts and affect patients' survival rates and outcomes severely. In this blog post, we will provide essential insights into HCC metastases and delve into the therapeutic options. Over 60% of patients with HCC are diagnosed in advanced stages, leading to an overall 5-year survival rate of 21%. However, this rate is between 60% and 70% in patients with early diagnosis who undergo liver transplants.[2] Patients diagnosed with advanced-stage HCC, defined by the presence of vascular invasion or extrahepatic metastases, have a poor prognosis with a median survival of less than 1 year. [3] Early detection of HCC is vital in increasing therapeutic opportunities and improving patients’ outcomes, and new diagnostic biomarkers are under investigation to enhance HCC screening.[4] Available treatments for HCC metastases depend on the tumor's location, the extent of the cancer, and the patient's general condition. Surgical resection, liver transplant, radiofrequency, and microwave ablation are all first-line treatments for tumors that have not spread to other body parts. Chemoembolization is commonly used and improves survival in asymptomatic patients with multifocal regional disease. [5] Systemic therapies, such as sorafenib and lenvatinib have been shown to be effective in prolonging survival rates and outcomes in patients with advanced HCC. These agents are multikinase inhibitors that block tyrosine kinases involved in angiogenesis, cancer development and growth, and tumor microenvironment regulation. They are used as first-line therapy in advanced HCC with contraindications to VEGF and immune checkpoint inhibitors. Immune checkpoint inhibitors are instead used together with bevacizumab in patients without contraindication. Alternative tyrosine kinase inhibitors, such as regorafenib, cabozantinib, and ramucirumab are used as second-line treatments.[6] Scientists are also researching new therapies for advanced HCC, including novel molecular-targeted therapies (such as STAT3 and CDK4 inhibitors) and immunotherapies to use as single agents or in combination. Several clinical trials are currently underway to investigate the efficacy and safety of these new therapies for advanced and metastatic HCC.[7] Hepatocellular carcinoma is a critical concern for clinicians and patients, given the cancer progression and severity. Validating new diagnostic biomarkers and developing new therapeutic approaches to overcome drug resistance will be paramount in improving patients’ survival and quality of life.
Hitting the Target: Latest Developments in Anti-Her2 Therapy
Human epidermal growth factor receptor 2 (HER2; ERBB2) has been shown to induce oncogenesis in several cancers, particularly breast and gastric cancers. HER2 is estimated to be overexpressed in ~20% of all breast cancers, and outcomes for these breast cancers were poor before HER2-targeted therapies[1]. Our understanding of mechanisms by which HER2 drives tumor growth and metastasis led to one of the first targeted therapies for treating HER2+ breast cancers. Here we highlight what is known about HER2 and oncogenesis. and how this information can be applied to the development of new targeted therapies. Gene amplification of the ERRB2 oncogene is one of the most common genetic defects detected in HER2+ tumors and typically causes overexpression of HER2 at the cell membrane[2]. HER2 proteins more readily dimerize with other HER2 proteins to form homodimers or with other ERRB members to form heterodimers. These complexes induce oncogenic signaling cascades, including MAPK and PI3K/AKT/mTOR, which cause cellular proliferation, angiogenesis, and resistance to apoptosis[3]. Due to the dominant role of HER2 in breast cancer, anti-HER2 antibodies were developed as one of the first targeted therapies. In 2006, clinical trial results of breast cancer patients treated with the anti-HER2 antibody trastuzumab showed significant improvements in progression-free survival and overall survival[4],[5]. Unfortunately, ~20-25% of metastatic breast cancer patients develop resistance to anti-HER2 therapies. More recent studies have focused on engineering new forms of anti-HER2 antibodies or developing HER1/2 inhibitors that can be used alone or in combination with other targeted therapies. The current standard of care for HER2+ breast cancer includes chemotherapy with adjuvant HER2-targeted therapies and endocrine therapy as indicated. Advances in targeted therapies are further improving treatment protocols. The next-generation anti-HER2 monoclonal antibody margetuximab targets the same HER2 epitope as trastuzumab and is modified in its Fc domain to improve antibody-dependent cellular cytotoxicity.[6] Margetuximab was approved by the FDA in December 2020 for the treatment of metastatic breast cancer in patients who had received prior HER2 therapies[7]. Two different bispecific antibodies have also been developed and are in clinical trials: ZW25 is a bispecific antibody that targets two different HER2 epitopes, and PRS-343 is a bispecific antibody that targets a HER2 epitope and the 4-1BB costimulatory immunoreceptor[8]. Bispecific antibodies are under development for breast cancer and other cancers because they exploit the property that antibodies have two epitope binding sites and can be engineered to better target a single molecule or crosslink multiple molecules, like HER2 and immune checkpoint molecules. Antibody-drug conjugates have also been evaluated as novel therapeutics that target HER2. Trastuzumab deruxtecan is an anti-HER2 antibody conjugated to a cytotoxic payload that is linked by a cleavable drug linker[9]. This treatment has been recently approved by the FDA and it shows superior targeting of cytotoxic drugs to HER2+ tumor cells and shows efficacy on individuals who have been treated previously with anti-HER2 mAbs. HER2-specific tyrosine kinase inhibitors have also been successful in treating HER2+ tumors, especially brain metastases because these drugs can cross the blood-brain barrier. Lapatinib, neratinib, pyrotinib, and tucatinib are four HER2-specific tyrosine kinase inhibitors used to treat HER2+ breast cancers. Lapatinib is an oral, irreversible small molecule HER1/HER2/HER4 TKI that was first approved in 2007 for the treatment of metastatic breast cancer[10]. Neratinib is a similar, orally available irreversible small molecule HER1/HER2/HER4 TKI that showed better efficacy against EGFR mutants and has been approved for use as an adjuvant therapy following trastuzumab treatment[11]. The development of resistance is also a problem for HER2-targeted TKIs, and pyrotinib is an experimental HER1/HER2/HER4 TKI under investigation as a potential new drug that is less prone to resistance[12]. Tucatinib is a TKI that is highly selective for HER2 approved for use in combination with trastuzumab and capecitabine in HER2+ breast and colorectal cancers, including patients with metastases and who have received previous anti-HER2 treatment[13]. HER2+ breast cancers continue to be challenging to treat due to resistance and metastasis. Combination therapies with antibodies and targeted inhibitors have dramatically improved survival in HER2+ breast cancer patients, but individuals who relapse continue to be faced with limited treatment options. New antibody-drug conjugates, bispecific antibodies, and targeted inhibitors are under investigation and hold the promise of better, more durable treatment options for patients. [1] Hudis CA. Trastuzumab--mechanism of action and use in clinical practice. N. Engl. J. Med. 2007 Jul 5;357(1):39-51. [2] Slamon DJ, Clark GM, Wong SG, Levin WJ, Ullrich A, McGuire WL. Human breast cancer: correlation of relapse and survival with amplification of the HER-2/neu oncogene. Science. 1987 Jan 9;235(4785):177-82. [3] Moasser MM. The oncogene HER2: its signaling and transforming functions and its role in human cancer pathogenesis. Oncogene. 2007 Oct 4;26(45):6469-87. [4] Romond EH, Perez EA, Bryant J, Suman VJ, Geyer Jr CE, Davidson NE, Tan-Chiu E, Martino S, Paik S, Kaufman PA, Swain SM. Trastuzumab plus adjuvant chemotherapy for operable HER2-positive breast cancer. N. Engl. J. Med. 2005 Oct 20;353(16):1673-84. [5] Smith I, Procter M, Gelber RD, Guillaume S, Feyereislova A, Dowsett M, Goldhirsch A, Untch M, Mariani G, Baselga J, Kaufmann M. 2-year follow-up of trastuzumab after adjuvant chemotherapy in HER2-positive breast cancer: a randomised controlled trial. Lancet. 2007 Jan 6;369(9555):29-36. [6] Rugo HS, Im SA, Cardoso F, Cortés J, Curigliano G, Musolino A, Pegram MD, Wright GS, Saura C, Escrivá-de-Romaní S, De Laurentiis M. Efficacy of margetuximab vs trastuzumab in patients with pretreated ERBB2-positive advanced breast cancer: a phase 3 randomized clinical trial. JAMA Oncol. 2021 Apr 1;7(4):573-84 [7] https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-margetuximab-metastatic-her2-positive-breast-cancer. [8] Kunte S, Abraham J, Montero AJ. Novel HER2-targeted therapies for HER2-positive metastatic breast cancer. Cancer. 2020 Oct 1;126(19):4278-4288. [9] Doi T, Shitara K, Naito Y, Shimomura A, Fujiwara Y, Yonemori K, Shimizu C, Shimoi T, Kuboki Y, Matsubara N, Kitano A, Jikoh T, Lee C, Fujisaki Y, Ogitani Y, Yver A, Tamura K. Safety, pharmacokinetics, and antitumour activity of trastuzumab deruxtecan (DS-8201), a HER2-targeting antibody-drug conjugate, in patients with advanced breast and gastric or gastro-oesophageal tumours: a phase 1 dose-escalation study. Lancet Oncol. 2017 Nov;18(11):1512-1522. [10] Ryan Q, Ibrahim A, Cohen MH, Johnson J, Ko CW, Sridhara R, Justice R, Pazdur R. FDA drug approval summary: lapatinib in combination with capecitabine for previously treated metastatic breast cancer that overexpresses HER-2. Oncologist. 2008 Oct;13(10):1114-9. [11] Minami Y, Shimamura T, Shah K, LaFramboise T, Glatt KA, Liniker E, Borgman CL, Haringsma HJ, Feng W, Weir BA, Lowell AM, Lee JC, Wolf J, Shapiro GI, Wong KK, Meyerson M, Thomas RK. The major lung cancer-derived mutants of ERBB2 are oncogenic and are associated with sensitivity to the irreversible EGFR/ERBB2 inhibitor HKI-272. Oncogene. 2007 Jul 26;26(34):5023-7. [12] Li Q, Guan X, Chen S, Yi Z, Lan B, Xing P, Fan Y, Wang J, Luo Y, Yuan P, Cai R, Zhang P, Li Q, Zhong D, Zhang Y, Zou J, Zhu X, Ma F, Xu B. Safety, Efficacy, and Biomarker Analysis of Pyrotinib in Combination with Capecitabine in HER2-Positive Metastatic Breast Cancer Patients: A Phase I Clinical Trial. Clin. Cancer Res. 2019 Sep 1;25(17):5212-5220. [13] Murthy RK, Loi S, Okines A, Paplomata E, Hamilton E, Hurvitz SA, Lin NU, Borges V, Abramson V, Anders C, Bedard PL, Oliveira M, Jakobsen E, Bachelot T, Shachar SS, Müller V, Braga S, Duhoux FP, Greil R, Cameron D, Carey LA, Curigliano G, Gelmon K, Hortobagyi G, Krop I, Loibl S, Pegram M, Slamon D, Palanca-Wessels MC, Walker L, Feng W, Winer EP. Tucatinib, Trastuzumab, and Capecitabine for HER2-Positive Metastatic Breast Cancer. N Engl J Med. 2020 Feb 13;382(7):597-609.
Prostate Cancer - Drivers of Genetic Mutations & Their Role in Disease Progression
Prostate cancer is one of the most common forms of cancer that affects the prostate gland in the male urogenital tract. Most prostate cancers are slow growing and are usually detected in individuals older than age 50. Although environmental factors contribute to the development of prostate cancer, risk is significantly associated with incidence among first-degree relatives. In recent years, several inherited and spontaneously mutated genes have been linked to prostate cancer. Here we highlight these findings and how they provide insight into the development of targeted prostate cancer therapies. Prostate cancer tumors are typically characterized by a wide range of genomic aberrations including somatic copy number alterations (SCNAs), structural rearrangements, and point mutations. Metastatic prostate tumors may have hundreds of these aberrations throughout the genome, but recent studies of primary prostate tumors have been critical to defining mutations associated with tumor development. Most primary prostate tumors have SCNAs, typically in the form of deletions that target a small area of the genome1. Deletions are often seen in the tumor suppressor genes BRCA2, NKX3.1, PTEN, and RB12. Structural rearrangements are another source of genomic variation observed in primary prostate tumors, for which the TMPRSS2:ERG rearrangement is most common and causes the androgen-responsive TMPRSS2 serine protease to drive expression of the ERG oncogene3. Other rearrangements have been linked to prostate cancer, including TMPRSS2 fusions with other ETS family members beyond ERG (ETV1 and ETV4)4. Some studies have suggested a link between ERG rearrangements and SCNA incidence, although it is not yet clear if rearrangements lead to destabilization of the genome and increased occurrence of SCNAs1. Somatic mutations occur on relatively high frequency primary prostate tumors, and this has been linked to mutations DNA mismatch repair proteins, tumor suppressors and oncogenes. The tumor suppressor TP53 is consistently identified as mutated in prostate tumors5. Mutations in the tumor suppressor genes BRCA1 and BRCA2 are well known for their association with breast and ovarian cancer but have also been linked to prostate cancer, and recent studies have shown that certain BRCA2 pathogenic sequence variants are associated with an elevated risk for aggressive prostate cancer6,7. PALB2 is a protein that interacts with BRCA2, and a recent study indicated that individuals who have certain PALB2 variants are more predisposed to aggressive forms of prostate cancer8. In addition, mutations in genes associated with DNA mismatch repair (MMR), such as MSH2, MSH6, and MLH1, are associated with greater prostate cancer risk9, and individuals with Lynch syndrome, which is caused by a germline mutation in one of these MMR genes, are also at greater risk of developing an aggressive form of prostate cancer10. One of the most important genes involved in prostate cancer progress is the gene expressing the androgen receptor (AR). Dozens of somatic mutations have been identified in the AR, and many of these mutations target the ligand binding domain11. Some prostate cancers can be treated successfully with drugs that inhibit AR signaling, such as enzalutamide, but resistance frequently occurs and is associated with worse outcomes. AR promotes prostate cancer cell survival by regulating several cellular programs. Although AR activity inhibition through androgen deprivation therapy (ADT) results in the suppression of AR-related pathways and durable clinical remission12, the disease may recur as castration-resistant prostate cancer (CRPC), typically with reactivated AR signaling. In this case, patients are treated with second-generation AR pathway inhibitors such as enzalutamide and abiraterone. Unfortunately, durable complete responses under these treatments are rare, and a substantial number of CRPC tumors progress under treatment despite loss of AR signaling. CRPC with AR-null phenotype are classified as tumors with diffuse small cell or neuroendocrine (NE) characteristics (SCNPC) or as double-negative (DNPC) phenotype that lacks both NE and AR activity13. A recently described genome-wide CRISPR-Cas9 screen was used to identify kinases that could be inhibited in the presence of enzalutamide. BRAF or downstream MAPK signaling molecules were identified as targets that could be co-inhibited with enzalutamide to improve overall therapeutic effects of these drugs14. Genomic alterations in prostate cancer are highly variable and can impact many critical cellular processes. By understanding which genes drive disease progression, potential therapeutic targets can be identified, and disease outcomes under different treatment regimens can be better predicted. [1] Taylor BS, Schultz N, Hieronymus H, et al. Integrative genomic profiling of human prostate cancer. Cancer Cell. 2010 Jul 13;18(1):11-22. [2] Wallis CJ, Nam RK. Prostate Cancer Genetics: A Review. EJIFCC. 2015 Mar 10;26(2):79-91. [3] Tomlins SA, Rhodes DR, Perner S et al. Recurrent fusion of TMPRSS2 and ETS transcription factor genes in prostate cancer. Science. 2005 Oct 28;310(5748):644-8. [4] Rubin MA, Maher CA, Chinnaiyan AM. Common gene rearrangements in prostate cancer. J. Clin. Oncol. 2011 Sep 20;29(27):3659-68. [5] Ecke TH, Schlechte HH, Schiemenz K et al. TP53 gene mutations in prostate cancer progression. Anticancer Res. 2010 May 1;30(5):1579-86. [6] Patel VL, Busch EL, Friebel TM, et al. Association of Genomic Domains in BRCA1 and BRCA2 with Prostate Cancer Risk and Aggressiveness. Cancer Res. 2020 Feb 1;80(3):624-638. [7] Oh M, Alkhushaym N, Fallatah S, et al. The association of BRCA1 and BRCA2 mutations with prostate cancer risk, frequency, and mortality: A meta-analysis. Prostate. 2019 Jun;79(8):880-895. [8] Wokołorczyk D, Kluźniak W, Stempa K, Rusak B, Huzarski T, Gronwald J, Gliniewicz K, Kashyap A, Morawska S, Dębniak T, Jakubowska A. PALB2 mutations and prostate cancer risk and survival. Br. J. Cancer. 2021 May 18:1-7. [9] Ritch E, Fu SY, Herberts C, Wang G, et al. Identification of hypermutation and defective mismatch repair in ctDNA from metastatic prostate cancer. Clin. Cancer Res. 2020 Mar 1;26(5):1114-25. [10] Haraldsdottir S, Hampel H, Wei L, et al. Prostate cancer incidence in males with Lynch syndrome. Genet. Med. 2014 Jul;16(7):553-7. [11] Ferraldeschi R, Welti J, Luo J, Attard G, de Bono JS. Targeting the androgen receptor pathway in castration-resistant prostate cancer: progresses and prospects. Oncogene. 2015 Apr 2;34(14):1745-57. [12] Heinlein CA, Chang C. Androgen receptor in prostate cancer. Endocr Rev. 2004;25(2):276–308. [13] Bluemn EG, Coleman IM, Lucas JM et al. Androgen receptor pathway-independent prostate cancer is sustained through FGF signaling. Cancer Cell. 2017;32(4):474–489. [14] Palit SAL, van Dorp J, Vis D, Lieftink C, Linder S, Beijersbergen R, Bergman AM, Zwart W, van der Heijden MS. A kinome-centered CRISPR-Cas9 screen identifies activated BRAF to modulate enzalutamide resistance with potential therapeutic implications in BRAF-mutated prostate cancer. Sci. Rep. 2021 Jul 1;11(1):13683. Subscribe to our Trends in Oncology Blog
The Benefits of Cell Line-Derived Xenograft Models for Preclinical Oncology Screening
Preclinical oncology research is a critical component in the development of new cancer therapeutics, and it is essential that drug candidates are carefully screened before they are tested in human clinical trials. One valuable tool in preclinical oncology research is the use of cell line-derived xenograft (CDX) models. In this blog post, we will explore the benefits of CDX models for preclinical oncology screening and how they can be used to improve our understanding of cancer and the development of new treatments. CDX models are created by implanting human cancer cells into immunocompromised mice. These cells develop into tumors that resemble their human counterparts and can be used to study the biology of cancer and test new treatments. One significant advantage of CDX models is that they are relatively easy and fast to establish, making them a cost-effective alternative to other preclinical screening models.[1] CDX models allow researchers to study the response of tumors to treatments in vivo, replicating the conditions of human cancer. Additionally, they can be used to evaluate the pharmacodynamics and pharmacokinetics (PD/PK) of candidate drugs. These models allow researchers to evaluate how drugs impact tumor growth over time, and how the drug is distributed throughout the body. This information is critical in determining the optimal dosing regimen for cancer patients.[2-4] CDX models have been widely used in preclinical research for several decades and can provide valuable insights into the underlying biology of cancer. Tumors grown in CDX models can be analyzed in depth to identify biological markers that can inform the development of targeted therapies. The use of CDX models can help researchers better understand the complexity of cancer and identify new therapeutic targets.[5-6] In conclusion, CDX models offer several advantages for preclinical oncology screening, including their ease of establishment, ability to replicate human conditions, and ability to provide insights into the biology of cancer. By incorporating CDX models into their preclinical screening strategies, researchers can more accurately predict the efficacy of cancer drugs and improve the development of new cancer therapies. 1. Long Y, Xie B, Shen HC, Wen D. Translation Potential and Challenges of In Vitro and Murine Models in Cancer Clinic. Cells. 2022 Nov 30;11(23):3868. doi: 10.3390/cells11233868. PMID: 36497126; PMCID: PMC9741314. 2. Qin L, Wang L, Zhang J, Zhou H, Yang Z, Wang Y, Cai W, Wen F, Jiang X, Zhang T, Ye H, Long B, Qin J, Shi W, Guan X, Yu Z, Yang J, Wang Q, Jiao Z. Therapeutic strategies targeting uPAR potentiate anti-PD-1 efficacy in diffuse-type gastric cancer. Sci Adv. 2022 May 27;8(21):eabn3774. doi: 10.1126/sciadv.abn3774. Epub 2022 May 25. PMID: 35613265; PMCID: PMC9132454. 3. Chen Y, Chen HN, Wang K, Zhang L, Huang Z, Liu J, Zhang Z, Luo M, Lei Y, Peng Y, Zhou ZG, Wei Y, Huang C. Ketoconazole exacerbates mitophagy to induce apoptosis by downregulating cyclooxygenase-2 in hepatocellular carcinoma. J Hepatol. 2019 Jan;70(1):66-77. doi: 10.1016/j.jhep.2018.09.022. Epub 2018 Oct 1. PMID: 30287340. 4. Kendsersky NM, Lindsay J, Kolb EA, Smith MA, Teicher BA, Erickson SW, Earley EJ, Mosse YP, Martinez D, Pogoriler J, Krytska K, Patel K, Groff D, Tsang M, Ghilu S, Wang Y, Seaman S, Feng Y, Croix BS, Gorlick R, Kurmasheva R, Houghton PJ, Maris JM. The B7-H3-Targeting Antibody-Drug Conjugate m276-SL-PBD Is Potently Effective Against Pediatric Cancer Preclinical Solid Tumor Models. Clin Cancer Res. 2021 May 15;27(10):2938-2946. doi: 10.1158/1078-0432.CCR-20-4221. Epub 2021 Feb 22. PMID: 33619171; PMCID: PMC8127361. 5. Oduwole OO, Poliandri A, Okolo A, Rawson P, Doroszko M, Chrusciel M, Rahman NA, Serrano de Almeida G, Bevan CL, Koechling W, Huhtaniemi IT. Follicle-stimulating hormone promotes growth of human prostate cancer cell line-derived tumor xenografts. FASEB J. 2021 Apr;35(4):e21464. doi: 10.1096/fj.202002168RR. PMID: 33724574. 6. Tang N, Cheng C, Zhang X, Qiao M, Li N, Mu W, Wei XF, Han W, Wang H. TGF-β inhibition via CRISPR promotes the long-term efficacy of CAR T cells against solid tumors. JCI Insight. 2020 Feb 27;5(4):e133977. doi: 10.1172/jci.insight.133977. PMID: 31999649; PMCID: PMC7101140.
