Trends in Oncology
Predicting ADC Efficacy Using IHC and NGS
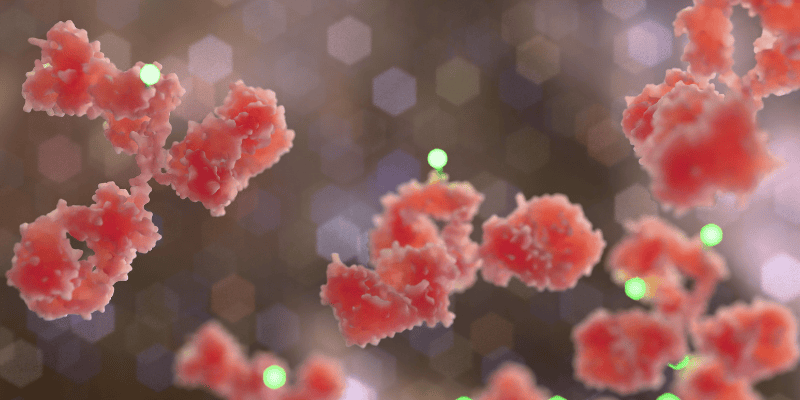
Antibody-drug conjugates (ADCs) represent a cutting-edge advancement in cancer therapy. These unique biopharmaceuticals act as "smart bombs," combining monoclonal antibodies specifically targeting cancer cells with potent cytotoxic drugs delivered directly to the tumor site. This precise targeting reduces collateral damage to healthy cells, minimizing adverse effects. Given the growing adoption of ADCs in clinical oncology, predicting their efficacy has become a critical challenge. Factors such as tumor heterogeneity, antigen expression, and individual patient differences underscore the need for precise biomarkers and advanced tools to determine patient suitability. The integration of immunohistochemistry (IHC) and next-generation sequencing (NGS) has emerged as a powerful approach to refining this prediction process. This blog explores the challenges of predicting ADC efficacy, the roles of IHC and NGS, and how these technologies are shaping the future of ADC-based therapy. The Importance of Predicting ADC Efficacy Why Predicting ADC Outcomes is Crucial? The therapeutic landscape of ADCs continues to evolve, with several FDA-approved ADCs and many others progressing through clinical trials. However, not all patients with cancer respond to these therapies, making the prediction of ADC efficacy vital to ensuring optimal outcomes. Key considerations include: • Target Antigen Expression: ADCs' performance depends on the presence and density of specific antigens on tumor cells. • Tumor Heterogeneity: Variability in antigen expression within and between tumors can impact ADC penetration and effectiveness. • Resistance Mechanisms: Both primary and acquired resistance to ADCs challenge their sustained efficacy. The Role of Immunohistochemistry in Predicting ADC Efficacy How IHC Works in ADC Therapy? Immunohistochemistry (IHC) is a gold standard for detecting protein expression within tumors. By applying antigen-specific antibodies to tissue samples, IHC enables visualization and quantification of target antigens. For ADCs, this method is highly valuable in determining whether a patient’s tumor expresses the antigen necessary for ADC binding and delivery. Benefits of Using IHC for ADC Target Assessment • Direct Visualization: Precise localization of target antigens not only confirms presence but also identifies antigen distribution within the tumor. • Threshold Analysis: IHC enables clinicians to set expression thresholds for ADC targeting, ensuring that only eligible patients receive therapy. • Readily Available Tool: IHC is widely accessible across pathology labs, making it a practical option for many cancer centers. Challenges in IHC Analysis Quantification of protein expression in IHC is typically assessed with H-scores, calculated by pathologists based on the identification of the percentage of cancer cells expressing the target and its level of intensity. The subjectivity of the methodology is an inherent risk of inconsistency for inter- intra- assay, for this reason, the H-score is usually calculated as the result of the independent IHC data analysis from at least two pathologists. Also, despite its benefits, IHC has limitations in predicting ADC efficacy, as for known ADC targets such as HER2 and TROP2, the correlation between target expression-related IHC scores and ADC efficacy, is not always strong. Next-Generation Sequencing (NGS) Contributions to ADC Accuracy What is NGS and How it enhances ADC Targeting? Next-generation sequencing (NGS) analyzes DNA, RNA, and gene expression at unprecedented speed and precision. By providing data-rich insights, NGS enables oncology researchers to evaluate molecular profiles in addition to traditional methods like IHC. In particular, NGS data can help researchers with the identification of biomarkers that may predict ADC responses. Recent studies have demonstrated NGS's advantages in ADC biomarker identification. For example, RNA sequencing correlations with IHC staining (e.g., TROP2, HER2) highlight strong alignment in certain targets, offering the potential for RNA-based cutoffs to complement IHC in ADC prediction. Variability, however, remains for some antigens, underscoring the need for continuing refinement. Innovations in Predicting ADC Efficacy Beyond IHC and NGS Emerging technologies and methodologies are refining ADC efficacy prediction even further. Key innovations include: • Multivariate Biomarkers: Next-gen tools like ADC Treatment Response Scores (ADC-TRS) evaluate gene expression alongside additional factors (e.g., adhesion, proliferation markers), significantly enhancing response prediction. • AI-Powered Pathology: Artificial intelligence in cancer pathology is enabling automated image and molecular data analysis, providing deeper insights into tumor heterogeneity and antigen expression thresholds. • Molecular Imaging: Imaging technologies are being integrated with NGS and IHC to provide real-time visualization of ADC biodistribution within patient tumors. Future Potential • Predictive Precision: Enhanced tools and algorithms will improve patient stratification, leading to better survival outcomes and fewer treatment-related toxicities. • Adaptive Therapies: With the ability to monitor antigen dynamics over time, clinicians can tailor ADC therapies to evolving tumor characteristics. Accurate Predictions Mean Better Outcomes for Patients Antibody-drug conjugates are paving the way for highly targeted and effective cancer treatments. However, maximizing their potential hinges on the ability to accurately predict suitable candidates through methods like IHC and NGS. By leveraging the latest advancements in predictive biomarkers and sequencing technologies, scientists and oncologists can improve patient outcomes, advancing precision medicine to new heights. As the field evolves, innovations will continue to refine ADC efficacy predictions, enabling personalized treatment strategies that benefit patients across diverse cancer types. Reach out to Champions Oncology to learn more about how we can help you develop your ADCs with our cutting-edge ex vivo and in vivo platforms and predictive tools that drive innovation. [1] Katrini J, Boldrini L, Santoro C, Valenza C, Trapani D, Curigliano G. Biomarkers for Antibody-Drug Conjugates in Solid Tumors. Mol Cancer Ther. 2024 Apr 2;23(4):436-446. doi: 10.1158/1535-7163.MCT-23-0482. PMID: 38363729. [2] Sachdev P. Thomas, Laurel A. Habel, Jennifer Marie Suga, Ninah Achacoso, Josh Nugent, Katarina M. Robinson, Ryan White, and Scott A. Tomlins. Evaluation of a predictive biomarker for antibody drug conjugates (ADCs). Journal of Clinical Oncology, Volume 42, Number 16_suppl. doi.org/10.1200/JCO.2024.42.16_suppl.3140 [3] Makawita S, Meric-Bernstam F. Antibody-Drug Conjugates: Patient and Treatment Selection. Am Soc Clin Oncol Educ Book. 2020 Mar;40:1-10. doi: 10.1200/EDBK_280775. PMID: 32213087. [4] Kushnarev V, Stupichev D, Kryukov K, et al143 Correlating RNA-seq detection and IHC staining of potential antibody-drug conjugate (ADC) targets: HER3, HER2, TROP2, Nectin4, and aFLRJournal for ImmunoTherapy of Cancer 2023;11:doi: 10.1136/jitc-2023-SITC2023.0143 [5] Ascione L, Crimini E, Trapani D, Marra A, Criscitiello C, Curigliano G. Predicting Response to Antibody Drug Conjugates: A Focus on Antigens' Targetability. Oncologist. 2023 Nov 2;28(11):944-960. doi: 10.1093/oncolo/oyad246. PMID: 37665782; PMCID: PMC10628585. [6] Paolo F. Caimi, Mehdi Hamadani, Carmelo Carlo-Stella, Masoud Nickaeen, Eric Jordie, Kiersten Utsey, Tim Knab, Francesca Zammarchi, Serafino Pantano, Karin Havenith, Ying Wang, Joseph Boni; CD19 Expression by IHC Alone Is Not a Predictor of Response to Loncastuximab Tesirine: Results from the LOTIS-2 Clinical Trial and Quantitative Systems Pharmacology Modeling. Blood 2022; 140 (Supplement 1): 9548–9550. doi: https://doi.org/10.1182/blood-2022-159626
Immunohistochemistry: a Powerful Tool in Cancer Research
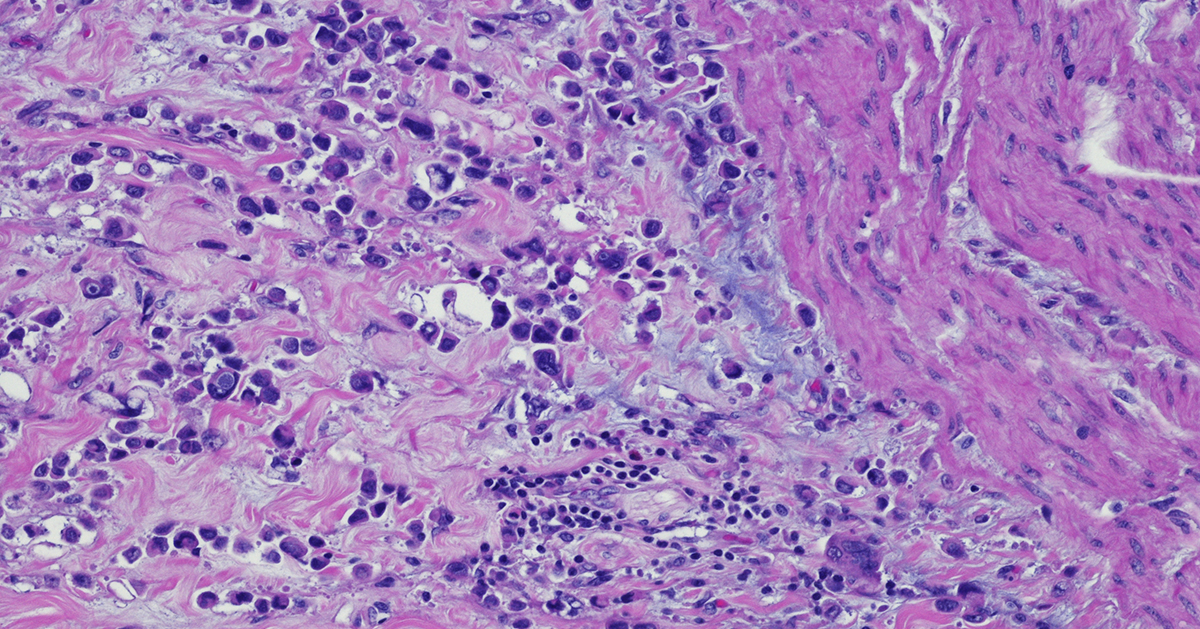
Immunohistochemistry (IHC) is a technique that originates in the early twentieth century but continues to be a valuable method that forms the backbone of molecular pathology. IHC is used for histological examination of tissues and specifically detects the presence of a molecule, such as a tumor antigen. IHC uses antibody-based labeling in which the primary antibody detects the target of interest and the secondary antibody detects the primary antibody which is linked to a molecule for microscopic visualization. Many different secondary antibody labeling modalities exist, including fluorescence, enzyme-mediated reactions and colloidal gold, and different labels are suited to specific microscopy platforms. Consider these five aspects of IHC as you implement this technique in preclinical cancer research: Quantitative measurements. IHC can be used as a qualitative measurement, but unlike many other visualization techniques, IHC can also be used as a quantitative measurement because antibodies that label specific parts of tissues or cells can be counted by a pathologist or with a computer-aided system. Developing robust validated quantitative IHC staining and visualization methods allows researchers to rely on the accuracy of this data. Customizable. IHC methods can be adapted to detect any cellular marker, given that a monoclonal antibody exists or can be made that specifically detects this marker. Validation of a new primary or secondary antibody also includes determining any off-target staining caused by these antibodies as this can be a critical determinant in the utility of an antibody. The ability to customize IHC in this manner is crucial to preclinical research that seeks to identify new biomarkers associated with tumor progression or immunotherapy efficacy. Flexibility. IHC can be used on almost any tissue type so long as it is processed correctly. Tissue samples from model animals as well as clinical biopsies can be fixed and sectioned in advance and stained at later times. Tumor microarrays (TMAs) can also be created and stained for evaluation of novel tumor markers or screening efficacy of drug candidates. This flexibility in sample type and handling highlights the overall utility of IHC. Automation. Currently, several different systems exist for automated IHC staining, and advances in digital analysis of IHC samples have allowed larger batches of clinical samples to be processed and evaluated. Comparison of automated IHC methods with manual methods has determined that these new approaches are accurate, sensitive, and reproducible. The big picture. Several methods exist for staining different targets in an IHC sample, and this allows scientists and clinicians to gain critical insights into which cells and molecules are present in the tumor microenvironment (TME), including levels of immune checkpoint molecules or infiltration of critical anti-tumor cell types. Consider how IHC can complement other techniques that look at the tumor microenvironment, including flow cytometry and RNAseq. IHC will continue to be a powerful tool in preclinical and clinical cancer research. Consider revisiting this classic technique as it has matured with the technological advances of the 21st century. Champions Oncology’s histology and immunohistochemistry services are custom developed and fully optimized to meet your needs in preclinical research. With industry leading pathology expertise and innovative automated technology, Champions provides you with the highest quality endpoints for your in vivo and ex vivo studies.

Leveraging IHC as a powerful clinical tool for IO therapies
Immunohistochemistry (IHC) is based on antigen–antibody binding to directly visualize the status of markers of interest in tissues. IHC provides a huge amount of information and is now indispensable in many fields including pathology, cancer biology, and drug discovery. IHC has been and continues to be analyzed by pathologists using microscopy. For pathologists in everyday practice or in the research context, IHC is an essential tool to interpret the pathophysiology of diseased tissues. Furthermore, IHC is also a crucial tool for biomarker discovery validation leading to personalized medicine. It provides information about the localization and the abundance of the target protein, both within tissue and at the sub-cellular level. More recently, growing evidence of the importance of spatial information enclosed in the tissue for patient stratification leading to improved clinical outcomes further boosted the development and standardization of many different and improved image analysis methods. This is particularly true in the field of immune-oncology and checkpoint inhibitors therapeutic development, where the presence of immune cells in the tumor correlated with positive clinical outcomes in many different types of cancer. IHC Analysis and Scoring Methods IHC results can be variable in both the percentage of positive detected cells as well as in protein expression intensity. The spatial distribution of the staining is also very variable. Sometimes the staining is widely spread out across the tissue while other times it is localized in small specific areas. The heterogeneity of the tissues reflected in the IHC staining needs to be classified, and more standardized scoring methods were needed to use this powerful tool in the clinic to stratify patients and improve outcomes. In fact, to have a diagnostic and prognostic value, the biomarkers detected by IHC need to be quantified and expressed in numerical values. Different methods have been developed to quantify IHC biomarker staining for diagnostic and therapy design. So far, a universally accepted standardized unbiased method to quantify IHC does not exist. Instead, for each tumor type and correlated therapeutic regimen a specific method with a defined antibody and protocol has been developed. The most common quantification methods are combinative semi-quantitative and percentage scoring methods.1 In the percentage scoring method, the relative immune-positive cell percentage in relation to the total number of cells is evaluated and reported using numbers from 0 to 9 where each unit increase represents 10% positive staining increments. For example, if the percentage of positive cells is between 0% and 9%, the score will be 0; if it is between 10% and 19%, the score will be 1; and so on. This method is preferable in large studies to avoid batch effects and can overcome interpretation errors in the evaluation of the positive cells. A limitation is that it does not include the staining intensity which in some cases could be important for patients’ stratification.2 Combinative semi-quantitative scoring is the most used method in the current prognostic biomarker research, providing a combined positive score incorporating both quantitative and qualitative assessments. In addition to the quantitative assessment of the relative immune-positive cell percentage described above, staining intensity is also assessed. Using the combinative semi-quantitative scoring method, the intensity is usually scored from 0 to 3 with 0 indicating negative staining, 1+ weakly positive staining, 2+ moderately positive, and 3+ strongly positive staining.2 Although IHC can be evaluated both quantitatively and qualitatively, an enormous number of variations is possible. This is due to the high number of diverse staining localization and spatial combinations. This leads to divergent interpretations among pathologists and discrepancies within pre-clinical and clinical studies evidencing the need for a more uniform system to interpret and quantify IHC data. Testing for PD-L1 in metastatic NSCLC PD-L1 expression is estimated in different manners depending on the type of cancer. Interestingly, in different indications, the presence of PD-L1 is not alone indicative of therapeutic efficacy. Different clinical trials demonstrated that, for different tumor types, PD-L1 localization correlated with treatment efficacy if PD-L1 is expressed in only immune cells, only cancer cells, or both. Thus, the IHC’s ability to localize the staining is fundamental.3 As an example of IHC use in the clinic, evaluation of PD-L1 expression helps identifying metastatic NSCLC patients who are eligible for treatment with pembrolizumab. In fact, in NSCLC, PD-L1 is a proven biomarker for patient response to pembrolizumab.3,4 In general, PD-L1 staining by IHC is evaluated using a combined positive score (CPS) and tumor proportion score (TPS) depending on the cancer type. The CPS score is calculated by counting the PD-L1 positive tumor cells and mononuclear inflammatory cells, then dividing this number by the total tumor cells, and multiplying by 100.4 CPS is used in the clinic to identify candidates for treatment with pembrolizumab in indications such as gastric cancer.3 In advanced NSCLC,4 the TPS scoring method is preferred to evaluate PD-L1 expression. TPS is calculated as the number of PD-L1 positive tumor cells divided by the total number of tumor cells and then multiplied by 100. Interestingly, to determine the eligibility of a patient for pembrolizumab treatment, only PD-L1 membrane staining is scored while staining intensity is not included in the score, and only the tumor cells and not the immune cells are evaluated. In this case, a competent, trained pathologist is critical to evaluate tumor heterogeneity and discriminate between tumor cells and infiltrating macrophages that are usually positive for PD-L1. For this PD-L1 staining scoring method to be reliable, at least 100 viable tumor cells must be evaluated within the patient’s tissue.2, 4 IHC has proven to be a powerful tool for oncology clinical practice. However, in order to fully leverage the information enclosed within the tissue in a clinical setting, and given the complexity of the IHC staining interpretation, crucial are both the pathologist’s training and expertise in the specific disease evaluation. [1] Dabbs DJ. 2014. Diagnostic immunohistochemistry: theranostic and genomic applications. 4th ed. Philadelphia: Elsevier Saunders. [2] Kim S, Roh J, Park C. 2016. Immunohistochemistry for Pathologists: Protocols, Pitfalls, and Tips, J Pathol Transl Med 50(6):411-418. [4] Inamura K. 2018. Update on Immunohistochemistry for the Diagnosis of Lung Cancer, Cancers10(3), 72; [3] Davis AA, Patel VG. 2019. The role of PD-L1 expression as a predictive biomarker: an analysis of all US Food and Drug Administration (FDA) approvals of immune checkpoint inhibitors, j. immunotherapy cancer 7, 278 .
