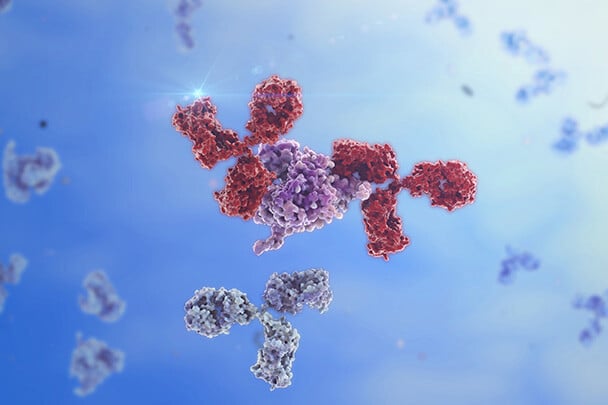
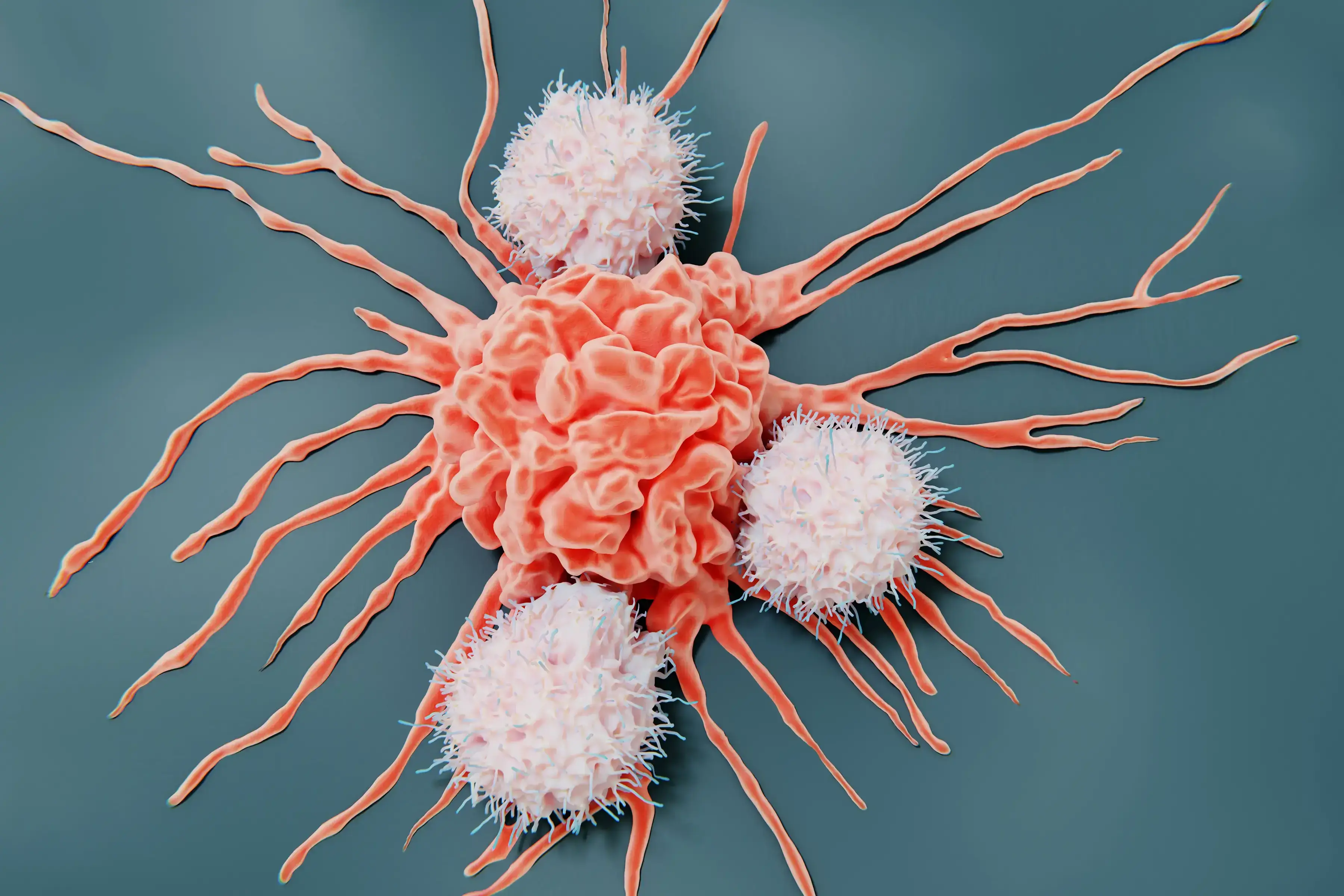
Bispecific antibodies represent a groundbreaking innovation in cancer immunotherapy. By binding to two distinct antigens simultaneously, these molecules direct immune cells to target cancer cells with precision, enhancing immune-mediated killing. The development of these therapies has opened new frontiers in oncology, with preclinical platforms playing a pivotal role in evaluating their efficacy, safety, and mechanisms of action before clinical trials.
History and Challenges of Bispecific Antibodies Research
The concept of bispecific antibodies originated in the 1960s, with the first experimental bispecific constructs developed in the 1980s using chemical cross-linking. Early versions were limited by instability and production challenges. Advances in genetic engineering in the 1990s led to the creation of more stable and functional bispecific molecules. Over time, the field has evolved to include trispecific, tetraspecific, and even pentaspecific antibodies, each designed to address specific therapeutic needs by engaging multiple targets or pathways simultaneously. The structural complexity of these molecules has grown, incorporating modular designs like dual-variable domain antibodies and Fc-engineered formats to enhance therapeutic efficacy and half-life. [1, 2]
The dual mechanisms of bispecific antibodies pose unique challenges in preclinical research. Traditional cell line-based models often fail to replicate the intricate interactions within the tumor microenvironment (TME), limiting their predictive power. Advanced models that closely mimic human tumor biology are required to fully understand the therapeutic potential and risks of bispecific antibodies.
Testing Bispecific Antibodies: In Vivo and Ex Vivo Approaches
Advanced preclinical models have been used to evaluate the performance of bispecific antibodies. Among the pre-clinical models, patient-derived xenografts (PDX) are invaluable for maintaining the genetic and histological fidelity of patient tumors. Representing the testing platform closer to the clinic, these models allow researchers to study tumor-specific responses and resistance mechanisms in vivo. Syngeneic models, using murine tumors in immunocompetent mice, provide insights into the immune system’s role in therapy efficacy. Yet, murine tumors and immune responses are very different from their human counterpart. While syngeneic models are a good proof of concept, they do not provide clinically translatable reliable data sets. [3]
Humanized mice incorporating human tumors together with human immune cells are very important in the field. The standard models used to test bispecific are adoptive transfer models leveraging peripheral blood mononuclear cells (PBMCs) or CD34+ stem cells. These systems replicate the interactions within the TME, enabling the study of immune cell recruitment, activation, and cytotoxicity driven by bispecific antibodies. The integration of humanized mouse models, engrafted with PBMCs or CD34+ stem cells, enhances the translational relevance of these studies by mimicking human immune responses more accurately. The use of humanized mice models can be challenging; however, the right expertise can help the selection of the best strategy for each bispecific MoA or combinatorial treatment of interest with CPI. [4]
Organoid models offer a controlled ex vivo environment to study complex cellular interactions, preserving the molecular diversity and histological characteristics of original patient tumors.
Adding immune cells to organoids generating a co-culture assay enables researchers to analyze interactions between cancer cells and immune cells within a reconstructed TME. These assays provide critical insights into immune cell recruitment and cytotoxicity, key to understanding bispecific antibody mechanisms of action. Co-culture systems offer a high-throughput, controlled environment for testing bispecific antibodies, maintaining tumor heterogeneity and complexity, making them ideal for pre-clinical interrogation of different strategies to address the complexities of bispecific antibody research.
In the hematologic malignancies field, leveraging primary, never-passaged, well-characterized patient material allows the evaluation of bispecific antibody efficacy in a clinically relevant ex vivo system where immune cell viability and function are retained.
Conclusion
The complexity of bispecific antibody mechanisms needs advanced preclinical platforms that accurately replicate human tumor biology, such as PDX in humanized in vivo hosts, organoids-based co-culture assays, and hematological platforms supporting immune cells, offering unparalleled tools for translational research. By integrating these platforms into bispecific antibody development, researchers can gain deeper insight into mechanisms of action, better predict therapeutic outcomes, and ultimately enhance clinical success.
The future of bispecific, trispecific, and even pentaspecific antibody therapies and the combination with checkpoint inhibitors hinges on the optimal selection and execution of specific translational strategies leveraging these innovative preclinical models.